Cold Medicine Safety Checker
Warning: This tool is for informational purposes only and does not replace professional medical advice. Always consult with your pharmacist or doctor before combining medications.
No dangerous interactions found
Your medications appear safe to take with this cold medicine. Always follow the recommended dosage and consult your pharmacist if you have concerns.
Dangerous interaction detected
What to do:
- Stop taking the cold medicine immediately
- Call Poison Control at 1-800-222-1222
- Visit emergency room if experiencing symptoms
Potential interaction warning
Recommendation:
- Consult your pharmacist before continuing
- Consider alternative medications without this ingredient
- Monitor for symptoms like dizziness, rapid heartbeat, or confusion
Every winter, millions of people reach for a bottle of cold and allergy medicine thinking they’re doing the right thing. They want relief-fast. But what they don’t realize is that many of these products are chemical cocktails, and mixing them can land you in the emergency room. You’re not alone if you’ve taken two different cold meds because you thought they were different. That’s exactly how 6.7 million Americans end up with too much acetaminophen every year, according to CDC data. And it’s not just about liver damage. The real danger is hidden in the labels, in the abbreviations, and in the way these drugs interact with each other-and with prescriptions you might already be taking.
What’s Actually in Your Cold Medicine?
Don’t assume that just because a product is sold over the counter, it’s harmless. Most combination cold and allergy meds contain four key ingredients, often in the same pill or liquid:
- Acetaminophen (also called APAP): For pain and fever. Found in Tylenol, DayQuil, NyQuil, and dozens of others.
- Pseudoephedrine or Phenylephrine: Decongestants that shrink swollen nasal passages. Pseudoephedrine works better but is kept behind the pharmacy counter. Phenylephrine is in most shelf brands like Sudafed PE and Tylenol Sinus.
- Dextromethorphan (DM): A cough suppressant. Common in Robitussin, Delsym, and Multi-Symptom Cold formulas.
- Chlorpheniramine or Diphenhydramine: Antihistamines that stop runny nose and sneezing. Also cause drowsiness-think Benadryl.
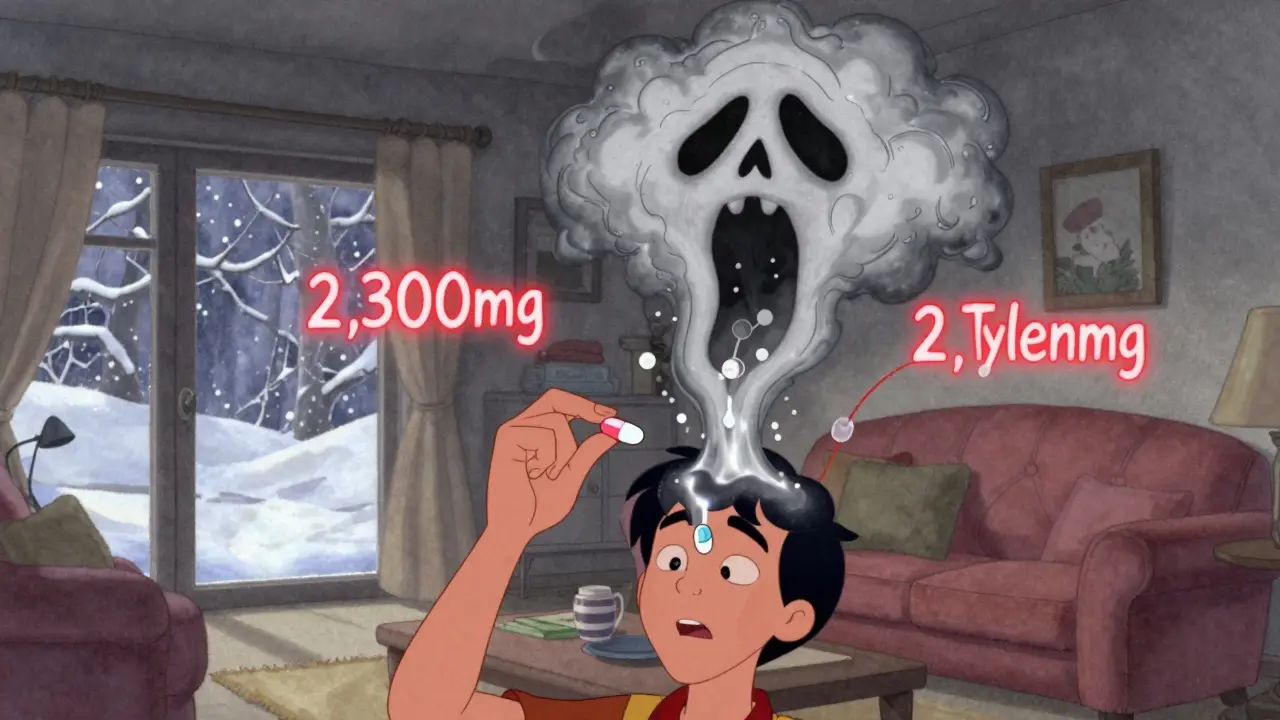
Here’s the problem: if you take a DayQuil for your cough and congestion, then take a separate pain reliever like Tylenol, you’re doubling up on acetaminophen. One bottle of DayQuil has 650mg. One regular Tylenol tablet has 500mg. Two of each? You’ve hit 2,300mg in a few hours. The daily limit is 4,000mg. But if you also take a nighttime cold med, you’re already over. And your liver doesn’t warn you until it’s too late.
Why Phenylephrine Might Be Doing More Harm Than Good
For years, phenylephrine was the go-to decongestant in OTC products because it didn’t require ID like pseudoephedrine. But here’s the truth: a 2022 review by researchers at the University of Florida and Rutgers found that 10mg of oral phenylephrine-what’s in most store brands-is no better than a placebo at clearing nasal congestion. Eleven clinical trials showed the same result.
Yet it’s still everywhere. Why? Because manufacturers replaced pseudoephedrine with phenylephrine to avoid sales restrictions. But here’s the twist: when phenylephrine is combined with acetaminophen, your body absorbs four times more of it than when taken alone. That’s not a coincidence-it’s a pharmacokinetic interaction. Higher levels mean higher risk. Studies show phenylephrine-acetaminophen combos increase the chance of high blood pressure, dizziness, and tremors by over 4 times compared to acetaminophen alone.
Meanwhile, pseudoephedrine still works. It reduces congestion by 65% on average. But it raises your blood pressure by 8-12mmHg and your heart rate by 5-8 beats per minute. If you have heart disease, uncontrolled hypertension, or take beta-blockers, it’s a bad idea.
The Silent Killer: Dextromethorphan and Antidepressants
Many people don’t know that dextromethorphan, the cough suppressant in cough syrups and cold pills, can interact dangerously with antidepressants. If you’re on an SSRI like sertraline (Zoloft) or an SNRI like venlafaxine (Effexor), mixing it with dextromethorphan can trigger serotonin syndrome-a rare but life-threatening condition.
Serotonin syndrome isn’t just feeling a little off. It means your body has too much serotonin, leading to:
- Fast heart rate
- High body temperature
- Agitation or hallucinations
- Muscle rigidity
- Seizures
A 2017 study in the Journal of Clinical Psychiatry found that combining dextromethorphan with SSRIs increases serotonin syndrome risk by 300%. And it’s not just prescription antidepressants. Some herbal supplements like St. John’s Wort and even certain migraine meds can do the same thing. If you’re on any mood stabilizer or antidepressant, check the label before taking anything labeled “DM.”
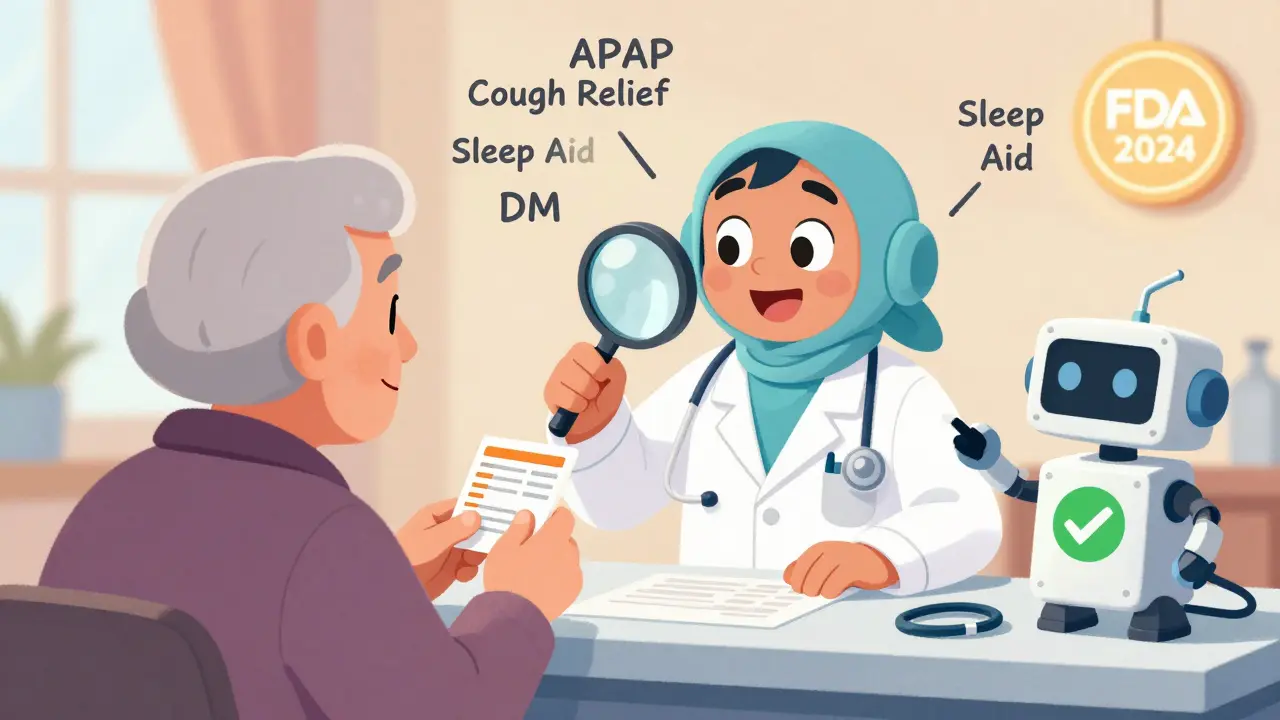
What You’re Not Seeing on the Label
Drug labels are designed to be confusing. You’ll see “APAP” instead of acetaminophen. “DM” for dextromethorphan. “PE” for phenylephrine. “CB” for chlorpheniramine. And if you’re not looking closely, you’ll miss it.
A University of Arizona study found that 68% of people don’t recognize “APAP” as acetaminophen. That’s why so many end up taking two products with the same ingredient. And even if you do read the label, the warnings are buried. The FDA now requires clearer labeling by December 2024, but right now, you’re on your own.
Here’s what you need to scan for every time you pick up a cold medicine:
- Is there acetaminophen? (Look for APAP)
- Is there a decongestant? (PE or pseudoephedrine)
- Is there dextromethorphan? (DM)
- Is there an antihistamine? (CB or diphenhydramine)
If you’re already taking a prescription for blood pressure, depression, or anxiety, you’re not just adding a cold pill-you’re adding risk.
When Combination Meds Are Okay (and When They’re Not)
Combination meds aren’t evil. They’re convenient. If you’ve got a full-blown cold-cough, congestion, headache, and runny nose-taking one product with all the right ingredients can be smart. But only if you’re not already taking something else with the same chemicals.
Here’s the rule: Only use combination products when you need all the symptoms treated. If you only have a stuffy nose, get a single decongestant. If you only have a headache, take plain acetaminophen or ibuprofen. If you’re allergic and just need to stop sneezing, take an antihistamine alone.
Using a multi-symptom pill for one symptom is like using a sledgehammer to crack a nut. You’re getting extra drugs you don’t need-and extra risks you didn’t sign up for.
And if you’re over 65, have kidney or liver disease, or take more than three medications daily? Avoid combination products entirely. Your body processes these drugs slower. The margin for error is razor-thin.
How to Stay Safe: A Simple 3-Step Plan
You don’t need to be a pharmacist to avoid a bad interaction. Just follow this:
- Read every label, front and back. Don’t just glance at the brand name. Look at the “Active Ingredients” section. Write them down if you have to.
- Check for duplicates. If you’re taking Tylenol for pain, don’t take NyQuil. If you’re on Zyrtec for allergies, don’t take a cold med with diphenhydramine. Both are antihistamines. You don’t need two.
- Ask your pharmacist. Walk into any pharmacy and say: “I’m taking X, Y, Z. I want to take this cold medicine. Is it safe?” They’ve seen this a thousand times. They’re trained for it. Don’t feel silly. This is exactly why they’re there.
And if you’re unsure? Use a free tool. The WebMD Drug Interaction Checker gets over a million checks a day. Or download Medisafe-it scans barcodes and tells you if you’re doubling up on anything.
What to Do If You’ve Already Overdosed
If you took too much acetaminophen-even if you feel fine-call Poison Control at 1-800-222-1222 immediately. Don’t wait for symptoms. Liver damage from acetaminophen can take 24-48 hours to show up. By then, it’s too late.
Signs of an overdose include:
- Nausea or vomiting
- Loss of appetite
- Sweating
- Pain in the upper right side of your abdomen
If you took dextromethorphan with an antidepressant and feel dizzy, confused, or your heart is racing-go to the ER. Don’t wait. Serotonin syndrome can kill in hours.
What’s Changing in 2026?
The FDA is reviewing phenylephrine’s effectiveness. If they decide it doesn’t work as a decongestant, manufacturers may have to reformulate or remove it from shelves. That could mean fewer combo products on the market-or stronger warnings.
Meanwhile, new labeling rules are coming. By the end of 2024, all combination cold meds must have high-contrast ingredient lists and bold warnings about duplicate ingredients. But until then, you’re the last line of defense.
Also, keep an eye on your prescriptions. If you’re on an SSRI, MAOI, or blood pressure med, talk to your doctor before using any OTC cold product. What’s safe for one person isn’t safe for another. Your medical history matters more than the brand name on the bottle.
There’s no magic pill for a cold. But there’s a smarter way to treat it. Skip the combo packs unless you need them. Choose single-ingredient options. Check every label. Ask questions. Your body will thank you.
Can I take allergy medicine with a cold medicine?
Only if you check the ingredients. Many allergy meds contain antihistamines like diphenhydramine or chlorpheniramine. Many cold meds do too. Taking both means you’re doubling your dose, which can cause extreme drowsiness, dry mouth, confusion, or even heart rhythm problems. Always compare the active ingredients before combining them.
Is it safe to take Tylenol with a cold medicine?
Only if the cold medicine doesn’t already contain acetaminophen. Most multi-symptom cold medicines like DayQuil, NyQuil, and Theraflu include acetaminophen. Taking Tylenol on top of that can lead to liver damage. Always check the label for “APAP” or “acetaminophen.” If it’s there, skip the extra Tylenol.
What’s the safest decongestant for high blood pressure?
If you have high blood pressure, avoid pseudoephedrine and phenylephrine entirely. Instead, try a saline nasal spray or a humidifier. For congestion relief without the risk, guaifenesin (an expectorant) is safe and helps loosen mucus. Always talk to your doctor before using any decongestant if you have heart disease or hypertension.
Can I take cold medicine if I’m on antidepressants?
Be very careful. Many cold medicines contain dextromethorphan, which can cause serotonin syndrome when mixed with SSRIs, SNRIs, or MAOIs. Symptoms include rapid heartbeat, confusion, fever, and muscle stiffness. If you’re on an antidepressant, avoid products with “DM” on the label. Ask your pharmacist for a safe alternative.
Why do some cold medicines make me feel jittery?
That’s likely the decongestant-either pseudoephedrine or phenylephrine. These work by narrowing blood vessels, which can raise your blood pressure and heart rate. That’s why you feel anxious, shaky, or like your heart is pounding. If this happens, stop the medicine and switch to a decongestant-free option. If symptoms persist, see a doctor.
Are natural remedies safer than OTC cold meds?
Not necessarily. Some herbal supplements like echinacea or zinc have limited evidence of benefit. Others, like St. John’s Wort, can interact with antidepressants and other medications. Honey and saline rinses are safe and helpful for cough and congestion. But don’t assume “natural” means “safe.” Always check with your doctor before mixing herbs with OTC or prescription drugs.
If you’ve ever felt worse after taking a cold medicine, you’re not imagining it. These products are powerful-and they’re not always as safe as they seem. The best way to protect yourself isn’t to avoid them entirely. It’s to understand what’s in them. Read the label. Know your meds. Ask questions. Your health isn’t a gamble.
