Tacrolimus-Azole Interaction Calculator
Calculate Your Tacrolimus Adjustment
Enter your current tacrolimus dose and select the azole you're prescribed to estimate potential interactions.
Your Results
Key Recommendations
- For Ketoconazole: Avoid completely in tacrolimus patients.
- For Voriconazole: Reduce tacrolimus by 50-75% before starting.
- For Posaconazole: Reduce tacrolimus by 50-75% before starting.
- For Isavuconazole: Reduce tacrolimus by 30-50% before starting.
- General: Monitor levels daily for first 3-5 days, then 2-3x weekly.
Why Azoles and Tacrolimus Don’t Belong Together
Imagine you’re a kidney transplant patient, taking tacrolimus every day to keep your new organ from being rejected. Then you get a fungal infection-maybe aspergillosis-and your doctor prescribes voriconazole, a powerful antifungal. Within days, your creatinine skyrockets. Your kidneys start failing. You’re rushed to the hospital. This isn’t rare. It happens weekly in transplant clinics across the U.S. and Europe.
The culprit? A silent, deadly interaction between azole antifungals and tacrolimus. It’s not a guess. It’s not theory. It’s well-documented, predictable, and preventable. Yet, too many patients still get caught in this trap.
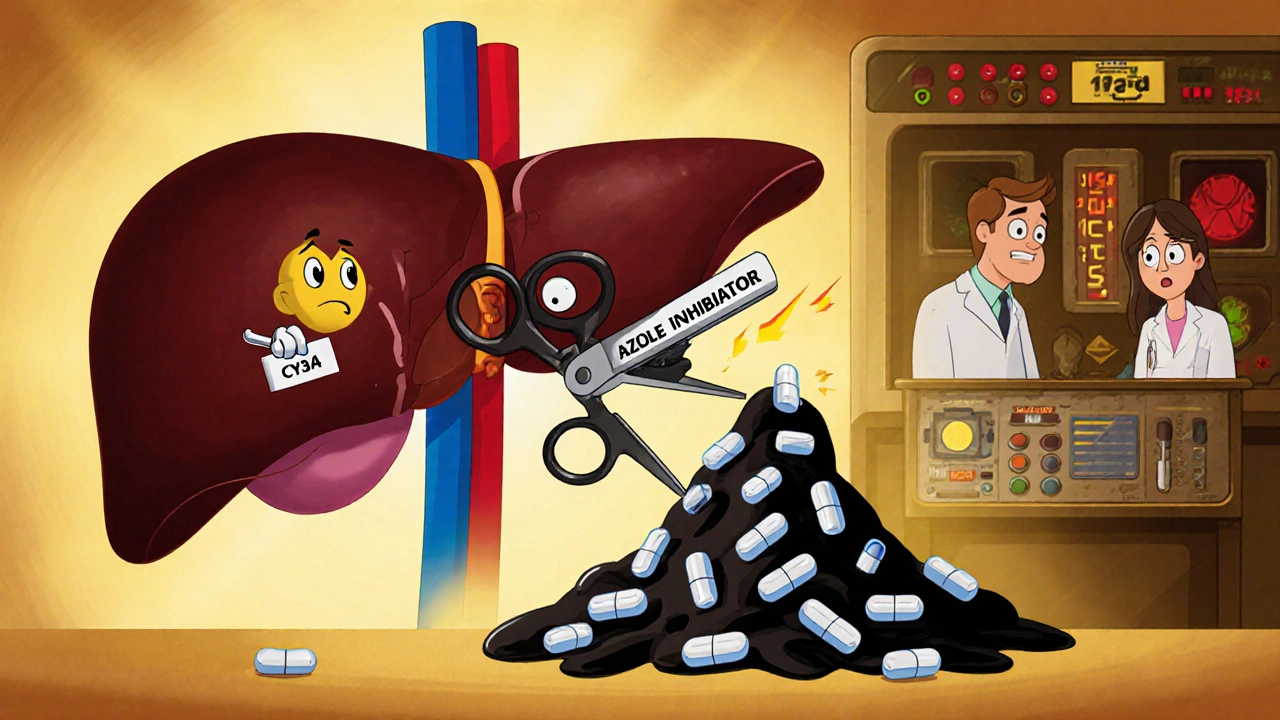
How the Interaction Works
Tacrolimus doesn’t stay in your body long. It’s broken down by enzymes called CYP3A4 and CYP3A5-mostly in your liver and gut. These enzymes are like tiny scissors, cutting tacrolimus into pieces so your body can flush it out. But when you take an azole antifungal-like ketoconazole, voriconazole, or itraconazole-those scissors get jammed.
Azoles are strong inhibitors of CYP3A4. They bind tightly to the enzyme and block it from doing its job. The result? Tacrolimus piles up in your blood. Levels can jump 2 to 10 times higher than normal. A patient with a stable level of 6 ng/mL can suddenly hit 18 ng/mL overnight. That’s not just a spike-it’s a warning sign of impending kidney damage.
According to data from the NCBI Bookshelf, over 95% of tacrolimus is cleared through bile, not urine. That means your liver is the main gatekeeper. When azoles shut down that gate, the drug doesn’t just linger-it accumulates to toxic levels.
Which Azoles Are the Worst?
Not all azoles are created equal. Some are like sledgehammers to CYP3A4; others are more like a gentle tap.
- Ketoconazole is the strongest inhibitor. It can boost tacrolimus levels by 300-500%. It’s so dangerous that most transplant centers ban it outright in CNI-treated patients.
- Voriconazole is next. It’s commonly used for aspergillosis and increases tacrolimus by 100-300%. Many patients don’t realize how fast this happens-levels can spike within 24-48 hours.
- Itraconazole and Posaconazole are moderate but still risky. They typically raise levels by 150-250%. Posaconazole is often used for prophylaxis in lung transplants, where fungal infections are common.
- Isavuconazole is the outlier. It’s a newer azole with much weaker CYP3A4 inhibition. Studies show it only increases tacrolimus by 30-50%. That’s why some centers are switching to it, even though it’s more expensive.
One transplant pharmacist in Leeds told me: “We used to use voriconazole for every lung transplant patient with fungal risk. Now we check if isavuconazole is covered by insurance first. If not, we cut tacrolimus to 25% of the original dose and monitor daily.”
The Cost: Nephrotoxicity and Kidney Damage
Tacrolimus isn’t just immunosuppressive. It’s directly toxic to the kidneys. It causes vasoconstriction in the tiny blood vessels of the glomeruli, reducing blood flow. Over time, this leads to chronic interstitial fibrosis and irreversible damage.
When levels spike due to azoles, the damage accelerates. Studies show that peak tacrolimus concentrations correlate more strongly with nephrotoxicity than trough levels. In one study, patients with levels above 15 ng/mL had a 70% higher risk of acute kidney injury compared to those under 10 ng/mL.
Real-world data from Johns Hopkins Hospital found that azole-tacrolimus interactions account for 15-20% of all tacrolimus-related kidney injuries. That’s not a side effect-it’s a direct drug interaction.
One patient on a transplant forum wrote: “My creatinine went from 1.1 to 2.4 in two days. I thought it was rejection. Turns out, it was the voriconazole. I spent a week in the hospital. My new kidney nearly died.”
What Do Experts Recommend?
The American Society of Transplantation (AST) and other major groups have clear guidelines:
- Avoid ketoconazole completely in tacrolimus patients.
- If you must use voriconazole or posaconazole, reduce tacrolimus dose by 50-75% before starting the azole.
- Monitor tacrolimus levels daily for the first 3-5 days, then 2-3 times per week until stable.
- Use isavuconazole or echinocandins (like micafungin) whenever possible-they’re safer.
Dr. David Paterson, who co-authored the landmark 1997 paper on this interaction, says: “The potential for drug interactions should be reviewed before antimicrobial agents are prescribed to patients treated with tacrolimus.” Simple. Direct. No room for error.
But here’s the problem: Not all hospitals follow this. A 2022 survey by the European Transplant Coordinators Association found that 25-30% of centers still report at least one severe toxicity case per year from this interaction.
Real-World Management: What Works
Centers that survive this interaction well have systems in place:
- Standardized protocols: At one U.S. transplant center, they now use a pre-filled order set: “Start posaconazole → reduce tacrolimus to 25% → check levels daily for 5 days.” This cut toxicity events by 60% since 2020.
- Electronic alerts: When a clinician orders voriconazole for a tacrolimus patient, the EHR pops up a warning with dose adjustment recommendations and monitoring schedules.
- Pharmacist-led monitoring: In 89% of transplant centers, pharmacists manage this interaction directly. They’re the ones checking levels, adjusting doses, and catching delays before toxicity hits.
One common complaint? Insurance. Isavuconazole is safer, but it’s 3-4 times more expensive than voriconazole. Many insurers won’t cover it as first-line. So patients get the riskier drug, and the burden falls on the transplant team to manage the fallout.
What’s Changing in 2025?
There’s new hope. In 2023, the FDA approved an extended-release version of tacrolimus. It smooths out the peaks and valleys in blood levels, which may reduce nephrotoxicity-even during interactions.
More importantly, research is moving toward personalized dosing based on genetics. About 50-60% of people of African descent carry a gene variant (CYP3A5*1) that makes them “expressers.” Their bodies break down tacrolimus faster. That means they might need higher doses and experience less dramatic spikes with azoles.
Meanwhile, some centers are now using the C/D ratio (concentration per dose) instead of just trough levels. This gives a better picture of how the body is handling the drug. Studies show this approach cuts nephrotoxicity by 22%.

What Should You Do?
If you’re a transplant patient on tacrolimus:
- Always tell your doctor about every medication you take-including OTC antifungals like clotrimazole or fluconazole (yes, even topical ones can matter).
- Ask: “Is this antifungal going to raise my tacrolimus level?”
- Know your baseline level. If you’re not sure, ask for a copy of your last lab result.
- If you’re started on an azole, expect more frequent blood tests. Don’t assume your doctor will call you-ask when the next level is due.
If you’re a provider:
- Don’t rely on package inserts-they’re outdated.
- Use UpToDate or AST guidelines. Update your order sets.
- Involve your transplant pharmacist early. They’re your best defense.
Final Thought: This Isn’t Just a Side Effect-It’s a System Failure
Transplant medicine has come a long way. 5-year survival for kidney transplants is now 87.8%. But we’re still losing patients to preventable drug interactions.
This isn’t about bad doctors. It’s about systems that move too slowly. It’s about cost barriers. It’s about assuming “everyone knows” how dangerous this is.
It’s not enough to know the science. You have to build the safety nets. Because when a patient’s kidneys fail after a transplant, it’s not just a medical complication. It’s a failure of care.
Can topical azoles like clotrimazole affect tacrolimus levels?
Yes, even topical azoles can cause interactions. While systemic absorption is low, studies have shown measurable increases in tacrolimus levels when high-dose, long-term topical ketoconazole or clotrimazole is used, especially over large areas or broken skin. Always inform your transplant team before using any antifungal cream, even if it’s over-the-counter.
How often should tacrolimus levels be checked when starting an azole?
Daily for the first 3-5 days after starting the azole, then 2-3 times per week until levels stabilize. Many centers use a protocol of checking levels at 24, 48, and 72 hours, then again on day 5 and day 7. Waiting longer than 72 hours risks missing a dangerous spike.
Is isavuconazole always better than voriconazole for transplant patients?
In terms of drug interaction risk, yes. Isavuconazole increases tacrolimus levels by only 30-50%, compared to 100-300% with voriconazole. However, cost and insurance coverage often limit its use. If isavuconazole isn’t available, reducing tacrolimus by 75% and monitoring closely is the next best option.
Can I stop tacrolimus if my levels get too high?
Never stop tacrolimus without direct guidance from your transplant team. Stopping it suddenly can cause acute rejection, which is often irreversible. Instead, reduce the dose under supervision and monitor levels closely. The goal is to find a safe balance-not to stop the drug.
Are there alternatives to azoles for fungal infections in transplant patients?
Yes. Echinocandins like micafungin and anidulafungin don’t inhibit CYP3A4 and are safe with tacrolimus. Lipid formulations of amphotericin B are another option, though they carry their own kidney risks. The choice depends on the type of infection, severity, and patient factors. Always consult your infectious disease or transplant team before choosing.
Next Steps for Patients and Providers
If you’re a patient: Write down your current tacrolimus dose and last level. Bring it to every appointment. Ask: “Is this new medication going to affect my transplant drug?”
If you’re a provider: Audit your center’s protocol. Do you have an electronic alert? Do you reduce tacrolimus before starting azoles? Are pharmacists involved? If not, start today. One change-like a pre-filled order set-can save a kidney.
This interaction is predictable. It’s preventable. And too many people are still paying the price for inaction.

Comments
Sophia Lyateva
lol so u mean the pharma giants DONT want us to know isavuconazole is cheaper n safer?? 😏 they got us all hooked on voriconazole just so they can charge 10x for the 'new' one... and dont even get me started on how the FDA approves these drugs like its a game of monopoly 🤡
On November 18, 2025 AT 19:23
AARON HERNANDEZ ZAVALA
this is actually really important info i didnt know topical azoles could do this too i used clotrimazole for a rash last year and my doc never said anything about checking levels maybe thats why my creatinine spiked... thanks for laying it out clear
On November 19, 2025 AT 09:20
Lyn James
Let me tell you something, and I mean this with the gravitas of someone who has stared into the abyss of modern medicine and seen its hollow core: this isn't just a drug interaction-it's a moral failure wrapped in a bureaucratic bow. We have the science, we have the guidelines, we have the tools-but we choose profit over protection, convenience over care, and insurance forms over human lives. The fact that a patient’s kidney fails because their insurer won't cover isavuconazole isn't a tragedy-it's a crime. And every doctor who prescribes voriconazole without demanding the safer alternative is complicit. We don't need more studies. We need courage. We need accountability. We need to stop pretending this is just 'medicine'-it's capitalism with a stethoscope.
On November 19, 2025 AT 16:41
Craig Ballantyne
The CYP3A4 inhibition profile of azoles is well-characterized, and the pharmacokinetic displacement of tacrolimus is a Class I interaction per the Lexicomp database. That said, the implementation gap between evidence and practice remains significant, particularly in resource-constrained settings where EHR alerts are either absent or overridden. The pharmacist-led model-while empirically validated-requires institutional buy-in and reimbursement structures that are not universally aligned with clinical best practice. Isavuconazole’s marginal inhibition profile makes it the preferred agent, but cost-benefit analyses must also account for downstream nephrotoxicity management costs, which often exceed drug acquisition expenses.
On November 20, 2025 AT 21:39
Victor T. Johnson
stop pretending this is complicated 🤬 if your hospital still uses voriconazole without dropping tacrolimus to 25% you're literally playing russian roulette with someone's new kidney. i've seen it happen. kidney gone. patient on dialysis. doctor says 'oops'. nope. that's not an error. that's negligence. and if your pharmacy won't cover isavuconazole? fight them. call the CEO. post it on social. this isn't science-it's survival. and if you're not screaming about this, you're part of the problem. 💥
On November 22, 2025 AT 09:30