What Is Bile Acid Diarrhea?
Bile acid diarrhea (BAD), also called bile acid malabsorption (BAM), is a hidden cause of chronic watery diarrhea that many doctors miss. It happens when too many bile acids - substances your liver makes to help digest fat - end up in your colon instead of being reabsorbed in the small intestine. These excess bile acids act like a laxative, forcing water into your colon and speeding up digestion. The result? Frequent, urgent, sometimes greasy stools that don’t respond to typical IBS treatments.
It’s not rare. About 1 in 4 people diagnosed with IBS-D (diarrhea-predominant irritable bowel syndrome) actually have BAD. Many spend years trying different diets, probiotics, or antidiarrheals before anyone tests for it. The good news? Once diagnosed, it’s one of the most treatable gut conditions out there.
Three Types of Bile Acid Diarrhea
BAD isn’t one-size-fits-all. There are three clear types, each with a different root cause:
- Type I: Caused by damage or removal of the terminal ileum - the last part of the small intestine where bile acids are normally absorbed. This happens after surgery (like bowel resection), in Crohn’s disease, or from radiation damage.
- Type II: The most common and mysterious type. No structural damage is found. Your body just makes too much bile acid or doesn’t reabsorb it well. This is what most people mean when they say “idiopathic BAD.”
- Type III: Triggered by other gut conditions like celiac disease, chronic pancreatitis, or even after gallbladder removal. The problem isn’t the ileum - it’s the chaos in the rest of the digestive system pushing bile acids out of balance.
Knowing your type helps guide treatment. Type I often needs stronger binders. Type II responds well to diet and standard binders. Type III requires fixing the root issue - like going gluten-free if celiac is involved.
How Is It Diagnosed?
There’s no simple blood test you can walk into your doctor’s office and get. But there are reliable methods - if you know what to ask for.
The gold standard is the SeHCAT scan, a nuclear medicine test that tracks how much bile acid your body retains after swallowing a tiny radioactive dose. If retention is below 15% after 7 days, you have BAD. The problem? It’s not available in most U.S. hospitals.
So doctors use alternatives:
- Serum C4 test: Measures a bile acid precursor. Levels above 15.3 ng/mL strongly suggest BAD. It’s fast, cheap, and increasingly used.
- FGF-19 blood test: This hormone tells your liver to stop making bile acid. Low levels (below 85 pg/mL) mean your body isn’t regulating bile production properly.
- Fecal bile acid test: Directly measures bile acids in stool. Accurate but requires a 48-hour collection and a specialized lab.
Many patients are misdiagnosed because their doctors don’t test for BAD. If you’ve had chronic diarrhea for more than 4 weeks - especially if you’ve had gallbladder surgery, Crohn’s, or been told you have IBS-D - ask your gastroenterologist about these tests. A 2023 study found that 35% fewer unnecessary colonoscopies were done when hospitals started routine BAD screening.
The Best Bile Acid Binders
Once diagnosed, treatment is straightforward: bind the extra bile acids before they reach your colon. Three medications do this well:
- Cholestyramine (Questran): The original binder. Works great - about 70% of patients see improvement within 2-3 days. But it’s chalky, gritty, and often causes constipation. Dose: 4 grams 1-2 times daily. Many patients quit because of taste.
- Colestipol (Colestid): Similar to cholestyramine but slightly less gritty. Still causes constipation in up to 25% of users. Dose: 5 grams 1-2 times daily.
- Colesevelam (Welchol): The newest and most tolerable. Comes in tablets or powder you mix with liquid. Only 5% report constipation. It’s also FDA-approved for cholesterol and type 2 diabetes, so many patients already take it for other reasons. Dose: 1.875-3.75 grams daily.
Most patients start with colesevelam because of better side effects. If it doesn’t work, switch to cholestyramine. Don’t give up after one try - finding the right binder and dose can take 2-4 weeks.
Important: Take binders 1 hour before or 4 hours after other medications. They can block absorption of vitamins (A, D, E, K), thyroid meds, and birth control pills.

Dietary Changes That Actually Work
Medication alone isn’t always enough. Diet plays a huge role - and you don’t need to go on a radical cleanse.
1. Cut fat to 20-40 grams per day. Fat triggers bile release. Less fat = less bile = fewer symptoms. That means avoiding fried food, fatty meats, creamy sauces, butter, and full-fat dairy. A 2022 study showed reducing fat below 30g/day cut stool frequency by 40%.
2. Add soluble fiber - psyllium husk. Take 5-10 grams daily, split into doses before meals. Psyllium binds bile acids like the medication does, but naturally. It also firms up stool. Clinical trials show a 35% drop in daily bowel movements.
3. Eat smaller, more frequent meals. Three big meals flood your system with bile. Five or six small meals spread the load. One Cleveland Clinic study found this reduced post-meal urgency by 25%.
4. Avoid triggers. Common ones include:
- Caffeine (coffee, tea, soda) - boosts colon movement by 15-20%
- Artificial sweeteners (sorbitol, xylitol) - draw water into the gut
- Spicy foods - irritate the colon in sensitive people
- Alcohol - speeds up digestion
Try a 4-week elimination diet. Remove all triggers, then reintroduce one at a time every 3 days. Track symptoms in a journal. Most people find 2-4 specific triggers that worsen their diarrhea.
What About the Specific Carbohydrate Diet (SCD)?
Some patients swear by the Specific Carbohydrate Diet - which cuts out complex carbs like grains, lactose, and sucrose. A 2019 survey of 200 BAD patients found 45% had better control on SCD. But it’s extreme. You’re cutting out bread, pasta, potatoes, and most sugars.
It’s not necessary for everyone. But if you’ve tried binders and low-fat diet and still struggle, it’s worth a 6-week trial under a dietitian’s guidance. Many find they can ease off it later once symptoms stabilize.
Real Patient Experiences
People with BAD share common stories:
- “I thought I had IBS for 7 years. My stool was always greasy and floated. When I started colesevelam, it was like a switch flipped. No more panic attacks before leaving the house.”
- “Cholestyramine made me constipated. I switched to Welchol, mixed it with apple juice - now I can eat dinner without worrying.”
- “I lost 12 pounds because I was scared to eat anything. Once I learned to eat small, low-fat meals with psyllium, I gained it back - and felt normal again.”
But there are struggles too. Colesevelam costs $350-$450/month without insurance. Some patients stop because of price. Others get discouraged when binders don’t work right away.
Support helps. The BAD Patient Support Group has over 1,200 members. The BAD Tracker app lets you log meals, symptoms, and meds - and spot patterns you’d never notice otherwise.
What’s Next for BAD Treatment?
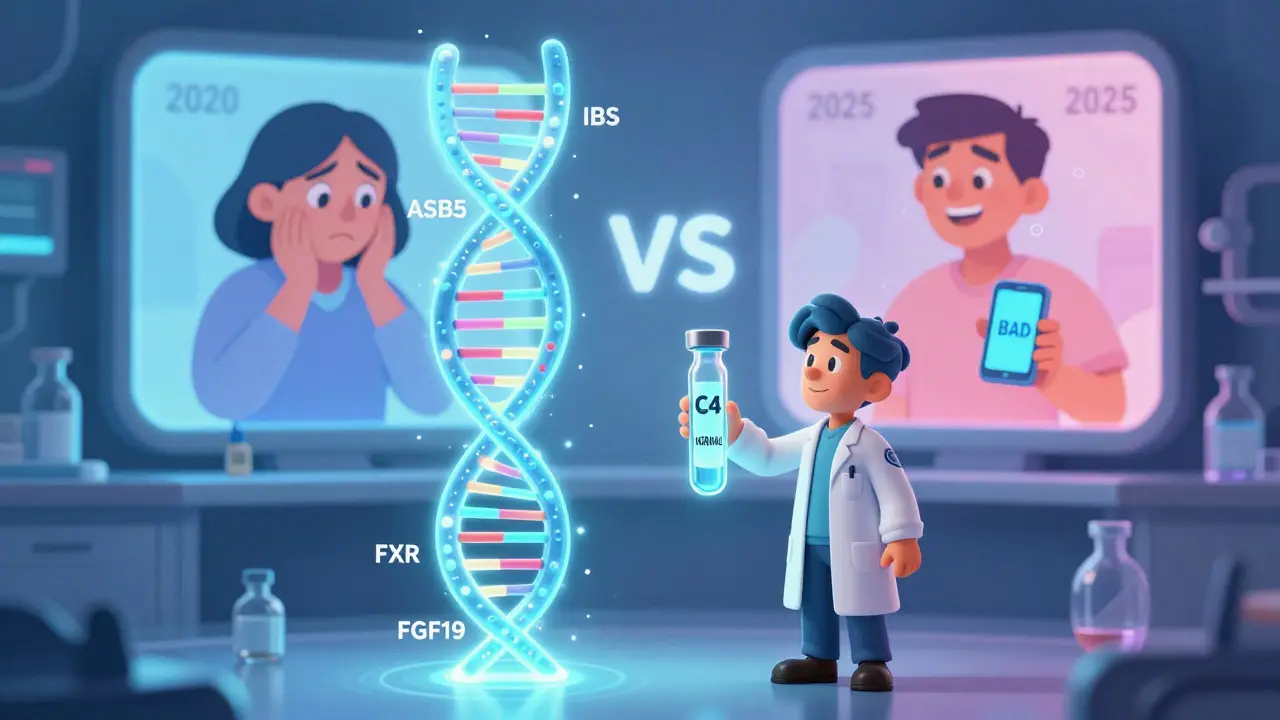
The future is promising. Researchers are developing drugs that target the bile acid regulation system directly:
- FGF19 analogs: These mimic the hormone that tells your liver to slow bile production. Phase 3 trials showed 72% symptom improvement - far better than binders.
- FXR agonists: These activate receptors that help reabsorb bile acids in the gut. Early results show fewer side effects than binders.
- Genetic screening: Four genes (TGR5, ASBT, FXR, FGF19) are linked to BAD risk. In the next 5 years, a simple blood test might tell you if you’re genetically prone.
By 2025, experts predict BAD will be officially separated from IBS-D in medical guidelines. Routine testing will become standard. Right now, only 15% of U.S. gastroenterologists test for it - but that’s changing fast.
When to See a Specialist
If you’ve had chronic diarrhea for more than 4 weeks - especially if:
- You’ve had gallbladder surgery
- You have Crohn’s disease or ileal resection
- You’ve been diagnosed with IBS-D but aren’t improving
- Your stools are pale, greasy, or float
- You have nighttime diarrhea or incontinence
Ask your doctor for a serum C4 test or refer you to a gastroenterologist who specializes in functional gut disorders. Don’t wait. BAD is treatable - and you don’t have to live with it.
Quick Summary / Key Takeaways
- Bile acid diarrhea causes chronic watery stool because too much bile reaches the colon - it’s not IBS.
- It affects up to 30% of people diagnosed with IBS-D, but is often missed.
- Diagnosis relies on blood tests (C4, FGF-19) or stool tests - ask for them if you have chronic diarrhea.
- Colesevelam (Welchol) is the best-tolerated bile acid binder; cholestyramine works but is harder to take.
- A low-fat diet (under 40g/day) plus 5-10g psyllium daily cuts symptoms by 35-40%.
Can bile acid diarrhea be cured?
It can’t always be “cured,” but it can be fully controlled. Most people achieve normal bowel habits with bile acid binders and diet. If BAD is caused by surgery or Crohn’s, lifelong management is needed. For idiopathic (Type II) cases, some patients can eventually reduce or stop binders after 1-2 years of stable diet control.
Do bile acid binders cause constipation?
Yes, especially cholestyramine and colestipol - up to 30% of users. Colesevelam causes constipation in only 5%. If you get constipated, lower the dose slightly and increase soluble fiber (psyllium). Drink more water. Don’t stop the binder without talking to your doctor - symptoms will return.
Can I take bile acid binders with other medications?
Not at the same time. Binders block absorption of many drugs, including thyroid meds, antibiotics, birth control, and vitamins A, D, E, and K. Take them 1 hour before or 4 hours after other medications. Always check with your pharmacist or doctor before combining.
Is a low-fat diet safe long-term?
Yes - if it’s balanced. You still need healthy fats (avocado, olive oil, nuts) for hormone and vitamin absorption. Aim for 20-40g total fat per day, mostly from plant sources. Avoid fried and processed fats. A registered dietitian can help you design a nutritionally complete low-fat plan.
Why do my stools look greasy and float?
That’s a classic sign of bile acid diarrhea. Bile helps break down fat. When too much bile floods the colon, it can’t be reabsorbed properly, and undigested fat ends up in your stool. This makes it oily, pale, and buoyant. It’s not fat malabsorption from pancreas problems - it’s bile overload.
Next Steps
If you suspect bile acid diarrhea:
- Track your symptoms for 2 weeks: frequency, stool appearance, triggers, timing.
- Ask your doctor for a serum C4 test - it’s the easiest first step.
- If positive, start colesevelam (Welchol) at 1.875g daily with food.
- Reduce dietary fat to under 30g per day. Add 5g psyllium husk before meals.
- Use the BAD Tracker app to log progress.
- Re-evaluate in 3 weeks. If no improvement, talk to a GI specialist about SeHCAT or FGF-19 testing.
You don’t have to live with constant urgency. BAD is treatable. You just need to ask the right questions.