Why Chemotherapy Safety Isn’t Just About the Patient
Chemotherapy isn’t just a treatment-it’s a powerful, toxic substance. If handled wrong, it can harm the person receiving it, the nurse giving it, or even the caregiver cleaning up after. The 2024 ASCO/ONS safety standards make this clear: every step, from the moment the drug leaves the pharmacy to when the patient goes home, must be controlled like a hazardous material spill. This isn’t alarmist. It’s science. And it’s backed by data from hospitals across the U.S.
Between 2018 and 2022, cases of cytokine release syndrome (CRS) from immunotherapy drugs jumped 300%. When CRS isn’t caught fast, mortality hits 12-15%. That’s why today’s protocols demand that antidotes like tocilizumab be immediately available at every treatment station. No exceptions. No excuses.
The Four Pillars of Safe Chemotherapy Administration
The 2024 ASCO/ONS standards break safety into four non-negotiable areas. Get one wrong, and the whole system weakens.
- Safe Environment: Facilities must use engineering controls like closed-system transfer devices (CSTDs) to prevent airborne exposure. Ventilation systems must be tested quarterly. Walls and surfaces must be non-porous and easy to decontaminate. This isn’t optional-it’s required by USP <800> in 48 U.S. states.
- Patient Consent and Education: Before treatment starts, patients must know exactly what drug they’re getting, why, how long it’ll last, and what side effects to watch for. This isn’t a form to sign-it’s a conversation. And it must be documented. No verbal agreements. No rushed explanations.
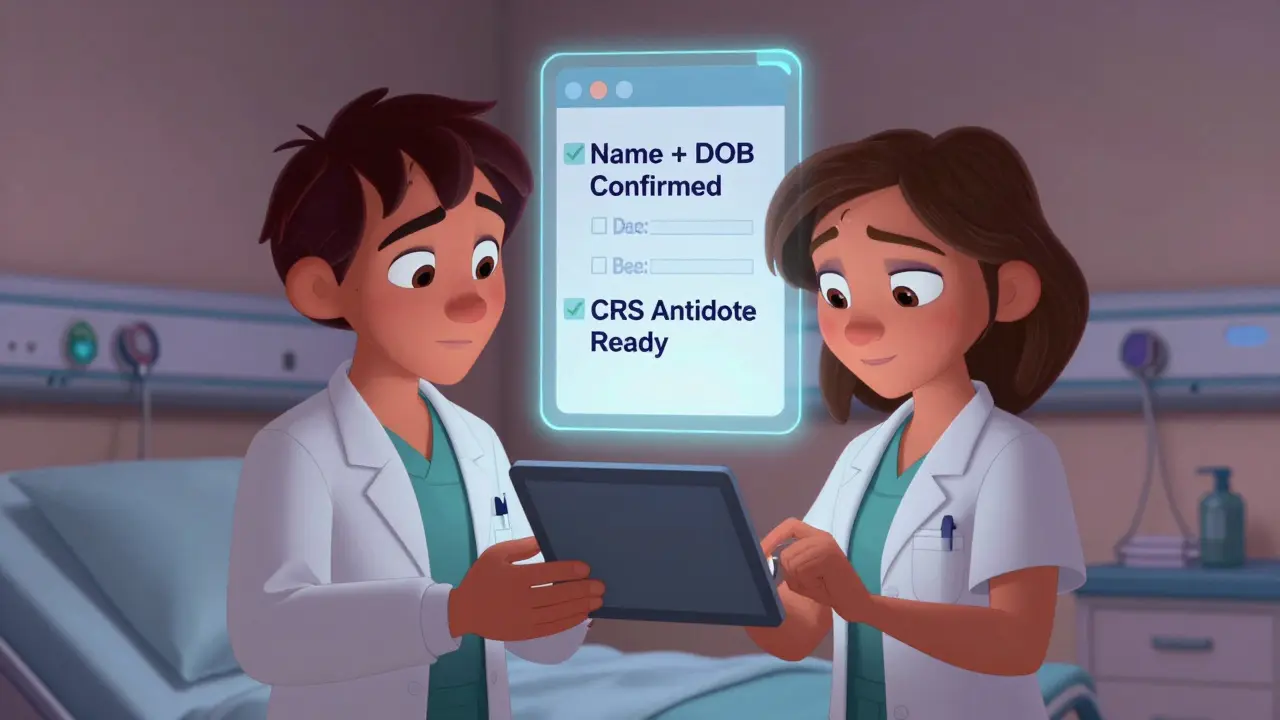
- Ordering, Preparing, Dispensing, Administering: This is where most errors happen. The 2024 update added a mandatory fourth verification step: two licensed clinicians must check the patient’s identity using two identifiers (name + date of birth) while standing at the bedside, right before the IV starts. This step alone reduced identification errors by 18% in NCCN’s 2022 safety database.
- Monitoring During and After: Patients must be watched for at least 30 minutes after infusion. Staff need to be trained to spot early signs of CRS-fever, low blood pressure, trouble breathing. If those signs appear, the protocol kicks in: stop the infusion, give oxygen, administer antidotes. Delay by even 10 minutes can be deadly.
Personal Protective Equipment: What Actually Works
Wearing gloves isn’t enough. You need the right gloves, tested for chemotherapy resistance. NIOSH and USP <800> require double gloving with chemotherapy-tested nitrile gloves-regular exam gloves can break down in minutes when exposed to drugs like carmustine or thiotepa.
Here’s what you need, every single time:
- Double chemotherapy-tested gloves (change every 30 minutes or if torn)
- Impermeable, disposable gown with closed back and tight cuffs
- Eye protection (goggles or face shield) if splashing is possible
- Respirator (N95 or higher) if aerosols are likely-like during IV bag changes or spill cleanup
And here’s what no one tells you: once you’ve handled chemo, your gloves are contaminated. Even if they look clean. Five studies since 1992 prove that contamination transfers from outer gloves to skin, surfaces, and even your phone. That’s why you never touch your face, your keys, or your clipboard without changing gloves first.
Home Chemotherapy: The Hidden Risk
More patients are getting chemo at home now. It’s convenient. But it’s dangerous if not done right.
The American Cancer Society found that 22% of home care incidents involve improper disposal of chemo waste. That means syringes, IV bags, even tissues with vomit or urine are being tossed in regular trash. One in five caregivers don’t know they need to wear gloves when cleaning up bodily fluids for 48-72 hours after treatment.
Here’s what home caregivers must do:
- Store all chemo drugs in a locked, child-proof container
- Use a dedicated chemotherapy spill kit (not just paper towels and bleach)
- Dispose of all used syringes, gloves, and bags in a FDA-cleared hazardous waste container
- Wash laundry separately, with gloves on, and run two full cycles
Facilities that use the ASCO-developed Chemotherapy Safety at Home toolkit cut caregiver safety concerns by 41%. That toolkit includes video guides, printable checklists, and a 24/7 nurse hotline. If your clinic doesn’t offer it, ask for it.
The Real Cost of Getting It Right
Implementing full safety protocols isn’t cheap. A medium-sized oncology clinic needs:
- $22,000-$35,000 in facility upgrades (CSTDs, ventilation, spill stations)
- $8,500-$12,000 for staff training and certification
- $4,200-$6,800 annually for PPE and hazardous waste disposal
- $15,000-$40,000 to modify EHR systems to support the four-step verification
But the cost of not doing it? Higher. Facilities with full compliance see 63% fewer medication errors and 78% fewer staff exposures. OSHA issued 142 citations for chemo safety violations in 2022-with an average fine of $14,250 per violation. That’s not just a fine. It’s a lawsuit waiting to happen.
And here’s the kicker: only 41% of nurses who are exposed to chemo actually report it. Fear of retaliation keeps them quiet. But unreported exposure means no tracking, no prevention, no accountability.

What’s Next: AI, Certification, and Equity
The future of chemo safety is here-and it’s changing fast.
By January 2025, the NCCN will require all accredited cancer centers to prove they’re doing the fourth verification step and have CRS protocols in place. If you’re not ready, you won’t be accredited.
Pilot programs are already testing AI systems that scan patient IDs, verify drug labels, and flag mismatches in real time. At 12 NCI-designated centers, these tools are cutting verification time from 10 minutes to under 2. That’s huge for nurses stretched thin.
But there’s a dark side. Dr. Sarah Temkin’s 2022 study found that 43% of rural clinics can’t afford CSTDs. That means patients in rural areas might get the same drugs-but not the same safety. This isn’t just a gap. It’s a health equity crisis.
By 2026, a national certification for chemo handlers is expected. Think of it like a CPR card-but for chemotherapy. You won’t be allowed to handle these drugs without it.
What You Can Do Today
Whether you’re a nurse, a caregiver, or a patient:
- Ask: “Do you use double gloves and CSTDs?”
- Ask: “Is there a CRS protocol here?”
- Ask: “Can I see the spill kit?”
- Ask: “Will you verify my name and birthdate at the bedside?”
If the answer is no, push. This isn’t about being difficult. It’s about staying alive.
Chemotherapy saves lives. But it can also take them-if safety is treated like an afterthought. The standards exist. The tools exist. The knowledge exists. Now it’s up to you to make sure they’re used.
What personal protective equipment is required for handling chemotherapy?
You must wear double chemotherapy-tested nitrile gloves, an impermeable disposable gown with closed back and tight cuffs, eye protection (goggles or face shield) if splashing is possible, and an N95 or higher respirator if aerosols could be created. All PPE is considered contaminated after use and must be disposed of properly.
What is the fourth verification step in chemotherapy administration?
The fourth verification step, mandated by the 2024 ASCO/ONS standards, requires two licensed clinicians to confirm the patient’s identity using two identifiers (like name and date of birth) while standing at the bedside, immediately before the chemotherapy infusion begins. This step was added to prevent fatal identification errors, which made up 18% of chemotherapy-related adverse events in 2022.
Why is CSTD important in chemotherapy handling?
Closed-system transfer devices (CSTDs) prevent hazardous drug vapors and droplets from escaping during preparation and transfer. They reduce staff exposure by up to 90% compared to open systems. CSTDs are now a core requirement in the ASCO/ONS 2024 standards and are mandated by USP <800> in most U.S. states.
Can chemotherapy be safely administered at home?
Yes, but only with strict protocols. Patients and caregivers must use dedicated chemotherapy spill kits, store drugs in child-proof containers, wear gloves when handling bodily fluids for 48-72 hours after treatment, and dispose of all waste in FDA-cleared hazardous containers. Facilities using the ASCO Chemotherapy Safety at Home toolkit report a 41% drop in caregiver safety concerns.
What should I do if I’m exposed to chemotherapy?
Immediately wash exposed skin with soap and water for at least 15 minutes. If eyes are exposed, rinse with water for 15 minutes. Remove contaminated clothing. Report the exposure to your supervisor and seek medical evaluation-even if you feel fine. Many effects are delayed. Never assume a small spill or glove tear isn’t serious.
How often should chemotherapy staff be trained?
Staff must complete 8-12 hours of initial certification training and then 4 hours of annual refreshers. Competency is verified through both a written exam (minimum 85% score) and a live observation of handling procedures. Training must be documented and kept on file.
What is cytokine release syndrome (CRS), and why does it matter?
Cytokine release syndrome (CRS) is a severe immune reaction triggered by some immunotherapies and newer targeted drugs. Symptoms include high fever, low blood pressure, trouble breathing, and organ dysfunction. If not treated immediately, mortality rates reach 12-15%. The 2024 standards now require facilities to have antidotes like tocilizumab and protocols ready before administering these drugs.
Troubleshooting Common Challenges
Problem: My facility says they don’t have time for the fourth verification step.
Solution: Track your near-miss errors for one month. Then show the data: the time saved by avoiding one error (like giving chemo to the wrong patient) is far greater than the 7-10 minutes added per dose. Use the Oncology Nursing Forum’s data: 52% fewer near-misses after implementing the step.
Problem: My home care patient refuses to wear gloves when cleaning up urine.
Solution: Give them the ASCO home safety toolkit. Show them the video on how chemo stays active in bodily fluids for 72 hours. Offer to send a nurse to demonstrate. If they still refuse, contact their oncology team-this is a safety violation.
Problem: I’m a nurse in a rural clinic. We can’t afford CSTDs.
Solution: Apply for state or federal grants for rural oncology safety upgrades. Many states have funds under the Cancer Prevention and Control Program. Don’t accept “we can’t afford it” as an answer. Patient safety can’t wait for perfect conditions.
