Chronic Kidney Disease Doesn’t Come With Warning Signs - Until It’s Too Late
Most people with early-stage chronic kidney disease (CKD) feel fine. No pain. No swelling. No obvious symptoms. That’s why nearly 7 in 10 cases go undetected until the kidneys are already badly damaged. By then, treatment options shrink, complications multiply, and the cost to the healthcare system spikes. But here’s the truth: if you catch CKD in its earliest stages, you can often stop it cold.
It’s not magic. It’s two simple tests - and knowing who needs them.
What Exactly Is Chronic Kidney Disease?
CKD isn’t just one disease. It’s a label for when your kidneys stop working the way they should - and it lasts for at least three months. Your kidneys filter waste, balance fluids, control blood pressure, and make red blood cells. When they’re damaged, these jobs get messy. The damage might come from diabetes, high blood pressure, genetics, or even long-term use of certain painkillers.
What makes CKD dangerous isn’t the damage itself - it’s how quiet it is. Unlike a heart attack or stroke, there’s no alarm bell. You won’t know something’s wrong until your kidneys have lost 50% or more of their function. That’s why diagnosis relies on lab tests, not how you feel.
The Two Tests That Save Kidneys (And Lives)
For years, doctors checked only one thing: serum creatinine. That’s a waste product your kidneys remove. But creatinine levels can be misleading. A person with low muscle mass - like an older adult or someone who’s very thin - might have normal creatinine even if their kidneys are failing. That’s why one test alone misses up to 40% of early CKD cases.
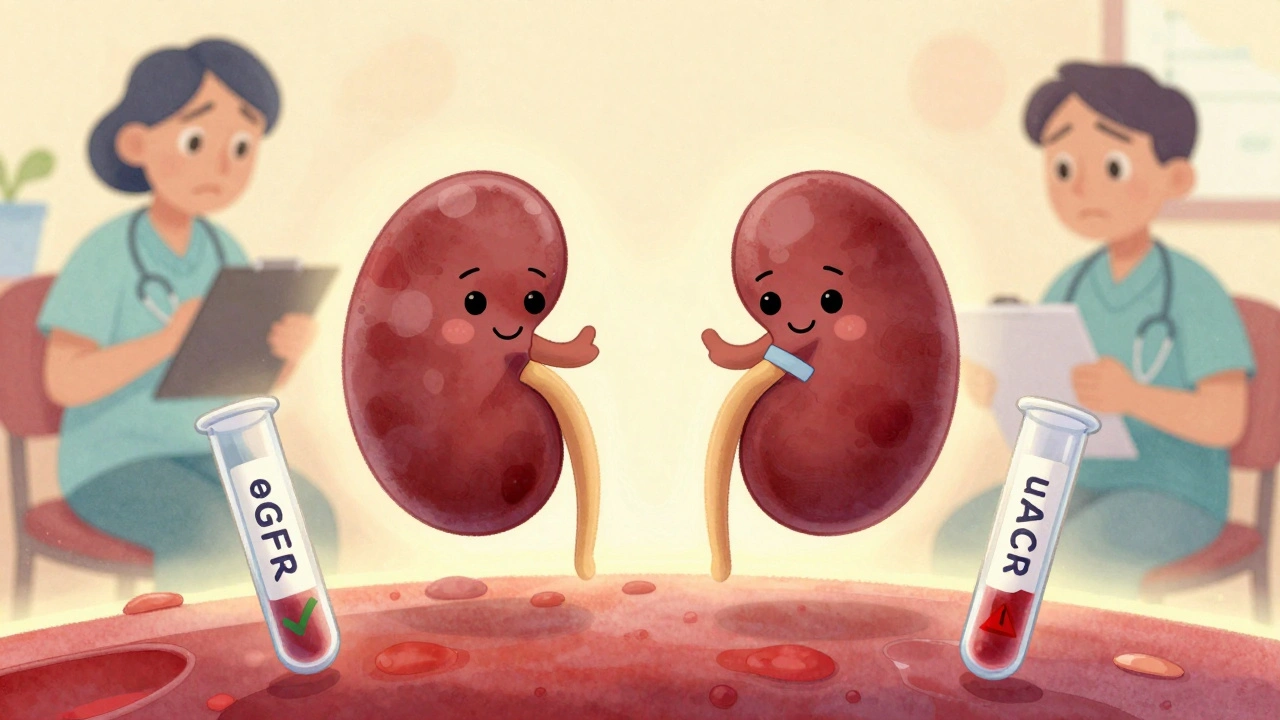
Today, guidelines from KDIGO and the National Kidney Foundation say you need two tests - and both must be abnormal for at least three months.
- eGFR - estimated glomerular filtration rate. This tells you how well your kidneys filter blood. It’s calculated from your blood creatinine, age, sex, and race. A normal eGFR is above 90. Below 60 for three months or more means CKD.
- uACR - urine albumin-to-creatinine ratio. This checks for protein (albumin) leaking into your urine. Healthy kidneys don’t let protein escape. If your uACR is 30 mg/g or higher, your kidneys are damaged - even if your eGFR is still normal.
This two-test rule is the biggest shift in CKD diagnosis since 2002. Before this, many people with early kidney damage were told they were fine. Now, if you have diabetes or high blood pressure and your uACR is high, you have CKD - even if your eGFR is 85.
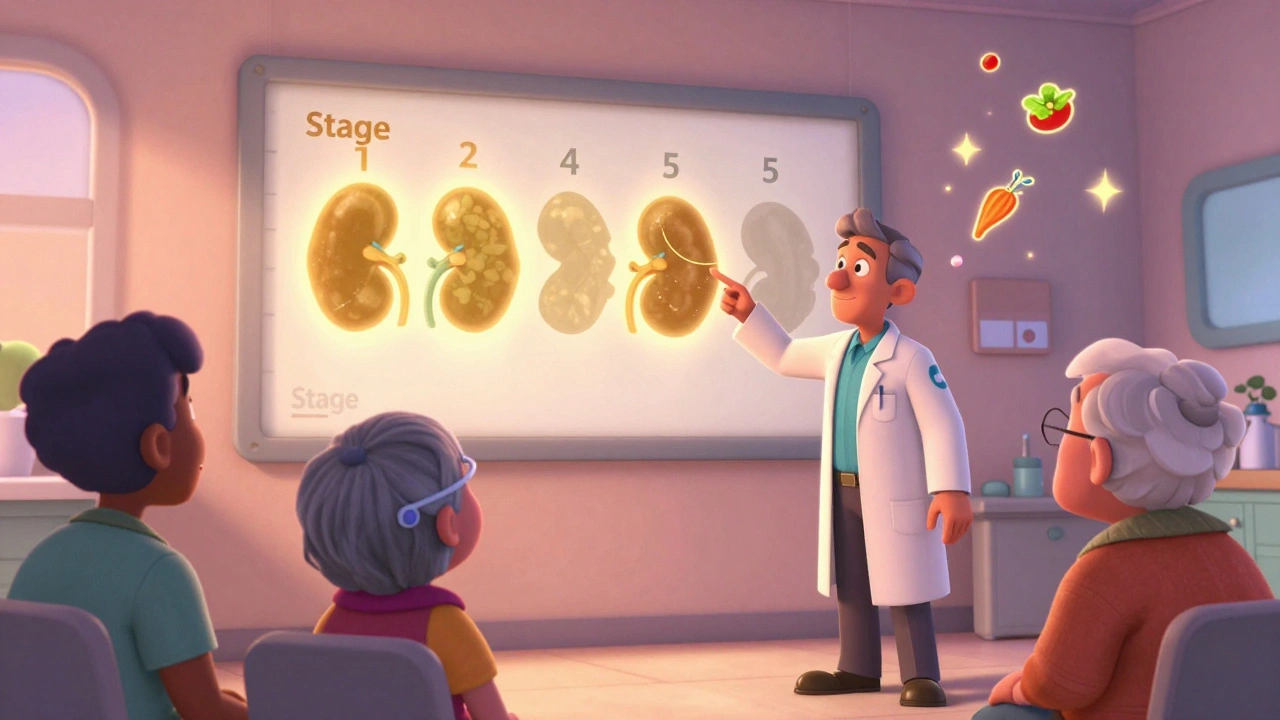
Understanding the Five Stages - And Why Stage 1 Matters Most
CKD is broken into five stages. But the first two stages are where the real window of opportunity opens.
| Stage | eGFR (mL/min/1.73 m²) | What It Means | Key Action |
|---|---|---|---|
| Stage 1 | 90+ | Normal kidney function, but signs of damage (uACR ≥30) | Find and treat the cause - often diabetes or high blood pressure |
| Stage 2 | 60-89 | Mild damage, still mostly working | Start medications like SGLT2 inhibitors or ACE inhibitors |
| Stage 3a | 45-59 | Mild to moderate loss | Monitor closely, adjust diet, control blood pressure |
| Stage 3b | 30-44 | Moderate to severe loss | Referral to nephrologist, prepare for possible dialysis |
| Stage 4 | 15-29 | Severe loss | Plan for dialysis or transplant |
| Stage 5 | <15 | Kidney failure | Start dialysis or get transplant evaluation |
Stage 1 and 2 are the golden window. If you’re caught here, you have a 5- to 7-year window to slow or stop progression. Studies show that with the right treatment, 60-70% of people never reach kidney failure.
Who Should Get Tested - And How Often
Not everyone needs annual screening. But if you fall into one of these groups, you should be tested every year - or even more often.
- People with type 2 diabetes - get tested at diagnosis. Then every year.
- People with type 1 diabetes - start testing five years after diagnosis, then annually.
- People with high blood pressure - check eGFR and uACR at least once a year. More often if your BP isn’t controlled.
- Those with a family history of kidney failure - get tested even if you feel fine.
- African Americans, Native Americans, and Hispanic populations - these groups have 2 to 4 times higher risk. Don’t wait for symptoms.
- People over 60 - kidney function naturally declines with age. Screening helps distinguish normal aging from true damage.
And here’s something most people don’t know: if you’re on long-term NSAIDs like ibuprofen or naproxen, or have autoimmune diseases like lupus, you’re also at risk. Ask your doctor.
How Early Intervention Actually Works
It’s not just about taking pills. It’s about a combination of smart medicine, lifestyle changes, and monitoring.
For example:
- SGLT2 inhibitors - originally diabetes drugs, they now reduce progression to kidney failure by 32% in people with CKD and albuminuria.
- ACE inhibitors or ARBs - these blood pressure meds also protect the kidneys by reducing protein leakage. Keeping your BP below 130/80 reduces progression risk by 27%.
- Diet - cutting salt, avoiding processed foods, and managing protein intake helps. A registered dietitian can help you build a kidney-friendly meal plan.
- Stopping smoking - smoking speeds up kidney damage. Quitting can slow decline by nearly half.
A 2022 meta-analysis found that patients who got full early intervention - medication, diet, education - saw their kidney function decline drop from 3.5 mL per year to just 1.2 mL per year. That’s a difference between reaching kidney failure in 10 years versus 30.
Why So Many People Still Get Missed
Even with clear guidelines, CKD is still underdiagnosed. Why?
A 2022 study found that only 53% of primary care doctors consistently order both eGFR and uACR for at-risk patients. In rural clinics, that number drops to 32%. Many still rely on creatinine alone.
Electronic health records often don’t remind doctors to order both tests. Patients don’t know to ask. And some doctors worry about overdiagnosing older adults - especially those over 85 with mildly low eGFR but no protein in their urine. That’s a real concern. Not every slight drop in eGFR is disease.
But the bigger problem? The U.S. Preventive Services Task Force says there’s “insufficient evidence” to recommend universal screening. That means insurance companies don’t always pay for it unless you’re already diabetic or hypertensive. That’s why millions slip through the cracks.

What’s Changing - And Why There’s Hope
Things are shifting. In 2023, the FDA cleared the first AI tool - NephroSight by Renalytix - that uses 32 data points to predict CKD risk before eGFR drops. It’s already being used in VA hospitals.
Medicare Advantage plans are now tying payments to how well they catch early CKD. Humana saw a 19% jump in early diagnoses after making dual testing mandatory.
And the Biden administration’s 2023 Executive Order is funding $150 million to implement universal dual-testing in federally funded clinics by 2026. That could identify over a million undiagnosed cases.
Even the way we calculate eGFR is changing. For decades, race was factored in - making Black patients’ kidney function appear better than it was. Newer formulas remove race, and early data shows this could increase early detection in African Americans by over 12%.
Your Next Steps - Even If You Feel Fine
If you’re in a high-risk group, here’s what to do now:
- Ask your doctor for an eGFR and uACR test - don’t wait for them to offer it.
- If you’ve had a creatinine test in the last year, ask if a uACR was done too.
- If your results are abnormal, ask for a repeat test in 3 months. One abnormal result isn’t enough.
- If you’re diagnosed with stage 1 or 2 CKD, ask about SGLT2 inhibitors or ACE inhibitors - even if your blood pressure is normal.
- Get connected with a dietitian who understands kidney health.
And if you’re not in a high-risk group? Talk to your doctor anyway. Kidney disease doesn’t care about your age, weight, or fitness level. It can sneak up on anyone.
Real Stories - Caught in Time
One Reddit user, u/KidneyWarrior2022, wrote: “My doctor only checked creatinine for 10 years. By the time they did uACR, I was stage 3.”
Another, u/PreventCKD, said: “Caught at stage 1 during a routine check-up. Five years later, still stage 1. Took the meds, changed my diet, and I’m still working full-time.”
That’s the difference between waiting - and acting.
Can you have chronic kidney disease with normal creatinine?
Yes. Creatinine alone is not enough. You can have normal creatinine but still have kidney damage shown by protein in your urine (uACR ≥30 mg/g). That’s stage 1 CKD. Many people are misdiagnosed because doctors only check creatinine.
Is CKD reversible?
The damage itself usually isn’t reversible. But progression can be stopped or slowed dramatically - especially in stages 1 and 2. With the right treatment, many people never reach kidney failure. The goal isn’t to fix the damage, but to stop it from getting worse.
Do I need a kidney biopsy if I’m diagnosed with CKD?
No, not usually. Most cases are diagnosed with eGFR and uACR alone. Biopsies are only done in 1-2% of cases - usually when the cause isn’t clear, or if there’s sudden worsening. For people with diabetes or high blood pressure, the cause is obvious, so biopsy isn’t needed.
Can lifestyle changes really help?
Absolutely. Cutting salt, avoiding processed foods, controlling blood sugar and blood pressure, quitting smoking, and staying active can slow decline by up to 65%. Diet and lifestyle aren’t optional - they’re the foundation of treatment.
Why does race matter in eGFR calculations?
Older formulas added a race adjustment that assumed Black patients had higher muscle mass, so their creatinine was naturally higher. That made their eGFR look better - even if their kidneys were damaged. Newer formulas remove race, leading to more accurate diagnoses, especially for African Americans. This change is now being adopted nationwide.
Are there any new tests coming soon?
Yes. The FDA is fast-tracking point-of-care uACR devices that give results in minutes - not days. These could be used in doctor’s offices, pharmacies, or even at home by 2025. AI tools that predict risk before kidney damage shows up are already in use in some clinics.
Final Thought: Don’t Wait for Symptoms
Your kidneys don’t scream. They whisper. And if you’re not listening - with the right tests - you might miss it until it’s too late. If you have diabetes, high blood pressure, or a family history of kidney disease, don’t wait. Ask for your eGFR and uACR today. Two tests. One chance to protect your future.
Comments
Jade Hovet
I got my uACR done last year after my doc finally stopped just looking at creatinine. Turned out I was stage 1 with diabetes. Took the SGLT2 inhibitor, cut out soda, and now my numbers are stable. 🙌 Don’t wait until you’re tired all the time - your kidneys don’t scream, they whisper. Listen.
On December 11, 2025 AT 06:25
Lauren Scrima
So… you’re telling me I should’ve asked for a test I didn’t know existed? Wow. Thanks for the guilt trip, doctor.
On December 12, 2025 AT 19:52
Donna Hammond
I work in a rural clinic, and I can tell you - most patients don’t even know what 'eGFR' stands for. We’ve started printing little cards with 'Two Tests = Early Save' on them. People grab them. They ask their PCPs. It’s small, but it’s something. If you’re over 50 and have high BP? Ask. Just ask. No shame. Your kidneys won’t remind you.
On December 14, 2025 AT 19:19
Richard Ayres
The shift from race-adjusted eGFR formulas represents a significant advancement in equitable clinical diagnostics. While some clinicians express concern regarding potential overdiagnosis in elderly populations, the data supporting early intervention in stage 1 and 2 CKD remains compelling. The integration of AI-driven risk prediction tools, such as NephroSight, further underscores the evolving paradigm of preventive nephrology.
On December 16, 2025 AT 04:49
Sheldon Bird
Man, I never thought my knee pain meds were hurting my kidneys. 😅 Got tested after reading this - uACR was through the roof. Switched to acetaminophen, started walking daily, and my doc put me on an ACE inhibitor. Feels good to be proactive. Still alive, still working. 🤘
On December 16, 2025 AT 14:18
Karen Mccullouch
They’re hiding this from us. Why? Because dialysis is a $100B industry. They want you sick. They don’t want you to know you can stop it with two tests. And don’t get me started on the race thing - they’re erasing Black biology to push a narrative. This is medical manipulation.
On December 17, 2025 AT 10:58
Michael Gardner
I’ve had a creatinine of 1.1 for 15 years. My doctor says I’m fine. You’re telling me I have stage 1 CKD? Then why does every single person I know over 50 have the same number? Is everyone in America secretly failing? Maybe the test is broken.
On December 17, 2025 AT 14:08
Willie Onst
Hey, I’m from the South and we don’t always trust doctors - but this? This made sense. My grandma had kidney trouble, never knew why. Now I’m making my whole family get tested. We’re gonna do it together. No more silence. 🤝
On December 18, 2025 AT 01:05
Ronan Lansbury
Ah yes, the classic 'Western medical establishment' narrative. How convenient that the FDA suddenly endorses an AI tool from a company with ties to pharmaceutical conglomerates. Meanwhile, in Germany, they use traditional herbal protocols with 87% success in early-stage CKD. But of course, you’d never hear that here.
On December 18, 2025 AT 17:45
Jennifer Taylor
I cried when I read this. I was stage 2 and didn’t know. My husband left me because I was always tired. My mom died of kidney failure at 58. I just found out I’m still stage 2. I’m on meds now. I’m eating clean. I’m alive. And if you’re reading this? You’re not alone. I’m fighting. Are you?
On December 20, 2025 AT 13:08
Shelby Ume
As a nephrology nurse educator, I’ve seen firsthand how devastating the delay in diagnosis can be. The two-test protocol is not merely a guideline - it is a standard of care. Patients who receive early education, dietary counseling, and pharmacologic intervention demonstrate significantly slower progression rates. I urge all clinicians to institutionalize this practice - and all patients to demand it.
On December 21, 2025 AT 14:51
nithin Kuntumadugu
lol why u think this works? u think ur kidney is like a phone? just update it? in india we use neem leaves and turmeric. no doctor. no test. no money. u think ur fancy lab test beat 5000 yrs of ayurveda? smh.
On December 22, 2025 AT 13:32
John Fred
SGLT2 inhibitors + ACEi + low-sodium diet + BP control = 70% reduction in progression. That’s not a guess - that’s a meta-analysis. If you’re diabetic and your doc isn’t talking about this, find a new doc. Period. 📈
On December 23, 2025 AT 09:07
Harriet Wollaston
I’m 34, no diabetes, no high BP, but my dad had kidney failure. I asked for the tests anyway. Stage 1. No meds yet - just diet changes and walking. I feel like I just unlocked a secret level in life. You don’t have to wait to be sick to care for your body.
On December 24, 2025 AT 04:23
sharon soila
The human body is a miracle of balance. When we neglect its quiet signals, we impose a cost not only on ourselves but on our families and communities. Early detection is not a luxury - it is an ethical imperative. Let us honor the dignity of health through vigilance, compassion, and action.
On December 24, 2025 AT 23:27
nina nakamura
You people are so dramatic. Everyone gets a little protein in their urine. It’s normal. You’re just scared of numbers. Go drink more water and stop Googling. Your kidneys are fine.
On December 25, 2025 AT 16:37
Hamza Laassili
I got tested after reading this. uACR was 45. Doc said 'it's nothing'. I said 'you're wrong'. I went to a nephrologist. He said I'm stage 2. Now I'm on meds. And I'm telling everyone I know. If you're not asking for both tests? You're not trying.
On December 27, 2025 AT 05:43
Rawlson King
I've seen too many patients get labeled with 'CKD' when they're just aging. You're turning normal physiology into pathology. This is medicine becoming a fear-based industry. Not every eGFR below 90 is disease. Some of us have lived well with 75 for decades.
On December 28, 2025 AT 10:08
Constantine Vigderman
I’m 68, type 2 diabetic, never had a uACR until last month. Was stage 1. Took the pill, started walking, lost 15 lbs. My eGFR’s still 88. I feel better than I have in 10 years. Don’t wait till you’re on dialysis to care. Do it now. 💪
On December 29, 2025 AT 18:41
Cole Newman
You know what’s wild? I’m a nurse. I’ve seen people die from this. But most of them? They didn’t know they were at risk. Your doctor didn’t tell you. Your mom didn’t tell you. You just assumed you were fine. Stop assuming. Ask. Now.
On December 31, 2025 AT 13:43