Hepatitis C is a viral infection that mainly harms the liver, but its impact reaches far beyond. Millions of people worldwide live with the virus, and many are unaware of the hidden dangers it poses to the heart. This article explains why hepatitis C matters for cardiovascular health, what the science says, and how you can protect your heart if you or someone you love carries the virus.
What is Hepatitis C?
Hepatitis C is caused by the hepatitis C virus (HCV), which spreads through blood-to-blood contact. Acute infection often shows no symptoms, while chronic infection can lead to liver fibrosis, cirrhosis, or liver cancer over years. The virus is diagnosed with a simple blood test that measures HCV antibodies and confirms active infection with RNA PCR. As of 2024, the World Health Organization estimates about 58 million people live with chronic hepatitis C globally.
Why Look at the Heart?
For decades doctors focused on the liver, but epidemiological studies started noticing that people with HCV had higher rates of heart attacks, strokes, and peripheral artery disease. The link isn’t a coincidence - the virus triggers systemic inflammation, alters lipid metabolism, and damages blood vessels, all of which are classic pathways to cardiovascular disease.
Key Mechanisms Connecting Hepatitis C to Heart Disease
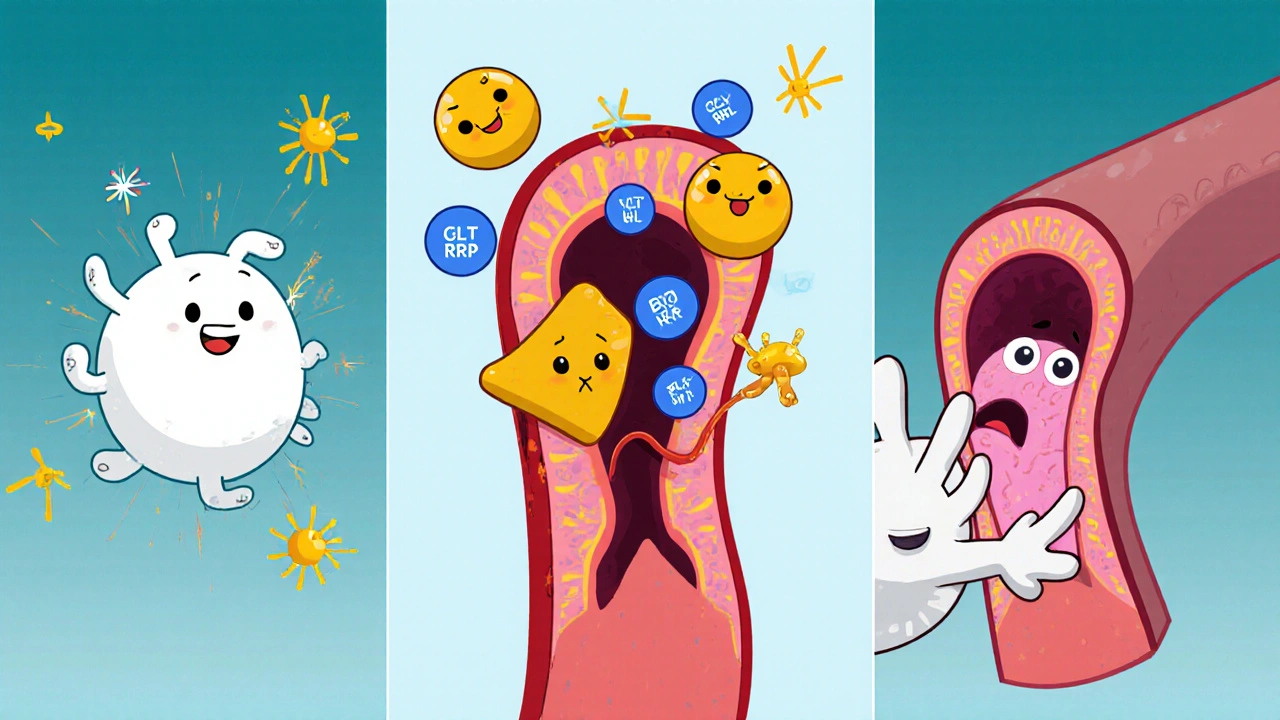
Three main biological processes help explain the connection.
- Chronic Inflammation: HCV keeps the immune system on high alert. Inflammatory markers such as C‑reactive protein (CRP) and interleukin‑6 stay elevated, encouraging plaque buildup in arteries.
- Liver‑Mediated Metabolic Changes: Damaged liver cells struggle to regulate cholesterol and triglycerides, often resulting in higher low‑density lipoprotein (LDL) and lower high‑density lipoprotein (HDL). This lipid imbalance fuels atherosclerosis.
- Endothelial Dysfunction: Direct viral presence in blood vessel walls can impair the endothelium’s ability to dilate, raising blood pressure and making clots more likely.
These mechanisms overlap with traditional heart‑disease risk factors, meaning HCV acts like an extra, hidden multiplier on your cardiovascular score.
Who Is Most at Risk?
Not everyone with hepatitis C will develop heart disease, but certain groups face higher odds.
- Older adults - age‑related stiffening of arteries compounds HCV‑induced inflammation.
- People with diabetes - both conditions share insulin resistance pathways.
- Heavy drinkers - alcohol accelerates liver damage, worsening lipid profiles.
- Individuals with hypertension - high blood pressure synergizes with endothelial dysfunction.
- Smokers - tobacco adds oxidative stress that magnifies viral inflammation.
What the Numbers Say
Several large‑scale cohort studies have quantified the added risk.
| Study | Population | Follow‑up (years) | Relative Risk (RR) | Key Outcome |
|---|---|---|---|---|
| NHANES (USA) 2018‑2022 | 12,500 adults w/ HCV | 5.2 | 1.68 | Myocardial infarction |
| EuroHeart (EU) 2016‑2021 | 8,300 chronic HCV | 4.8 | 1.45 | Ischemic stroke |
| Japanese Cohort 2015‑2020 | 5,200 HCV‑positive | 6.0 | 1.52 | Peripheral artery disease |
Across these studies, having hepatitis C raised the chance of a major cardiovascular event by roughly 45‑70 % after adjusting for age, smoking, diabetes, and hypertension.

How Antiviral Treatment Changes the Picture
Enter direct‑acting antivirals (DAAs). Since 2014, DAAs have cured over 95 % of patients with an 8‑week regimen. Research published in 2023 showed that achieving a sustained virologic response (SVR) lowered CRP levels by an average of 30 % and reduced the relative risk of heart attacks to near baseline within three years.
Key takeaways for anyone on DAA therapy:
- Continue routine cardiovascular screening - curing the virus doesn’t erase years of damage.
- Adopt heart‑healthy habits (diet, exercise, quit smoking) to maximize the benefit of viral clearance.
- Discuss with your hepatologist whether statins are safe; most modern studies suggest they are well‑tolerated alongside DAAs.
Managing Heart Health While Living with Hepatitis C
Here’s a practical checklist you can follow.
- Get Tested: If you haven’t been screened for HCV, ask your doctor for a blood test. Early detection opens the door to cure.
- Cardiovascular Risk Assessment: Ask for a lipid panel, blood pressure check, and a baseline ECG. Keep a record of CRP if your doctor orders it.
- Lifestyle Upgrade: Aim for at least 150 minutes of moderate aerobic activity per week, swap processed carbs for fiber‑rich vegetables, and limit alcohol to the recommended guidelines (no more than 14 units per week for men, 7 for women).
- Start Antiviral Therapy if eligible. The standard 8‑week DAA course is often enough; discuss side‑effects and drug interactions.
- Medication Review: If you have high cholesterol or blood pressure, ensure your meds don’t clash with DAAs. Many statins (e.g., pravastatin) are safe.
- Regular Follow‑up: After SVR, schedule a cardiovascular check‑up every 12‑18 months to catch any lingering issues early.
Following this plan helps cut the double burden of liver and heart disease, giving you a better chance at a long, active life.
Common Questions About Hepatitis C and Heart Disease
Does curing hepatitis C remove the heart disease risk?
Curing the virus lowers inflammation and improves lipid levels, which reduces risk. However, any damage that occurred before cure may persist, so ongoing heart‑health monitoring is still advised.
Can I take statins while on antiviral medication?
Most modern DAAs are compatible with statins like pravastatin and rosuvastatin. Your doctor will pick the safest option based on your liver function.
Is the increased heart risk the same for every genotype of HCV?
Current data suggest the risk is similar across genotypes 1‑4, the most common worldwide. Rare genotypes haven’t been studied enough to draw firm conclusions.
Do lifestyle changes matter if I’m waiting for treatment?
Absolutely. Improving diet, exercising, quitting smoking, and controlling blood pressure can lower the immediate cardiovascular threat while you arrange antiviral therapy.
What symptoms might hint at heart problems in a hepatitis C patient?
Typical heart‑attack signs apply: chest pressure, shortness of breath, sudden fatigue, or unexplained sweating. Because HCV patients often feel “tired” from liver issues, any new or worsening symptom deserves prompt medical review.
Understanding the link between hepatitis C and heart disease empowers you to act early. With modern antivirals, lifestyle tweaks, and regular heart checks, you can protect both your liver and your ticker.
Comments
Rachel Nimmons
they’re telling you it’s the virus… but what if the virus is just a symptom? what if the real problem is the toxins in our water, the vaccines, the 5G towers messing with your endothelial cells? they don’t want you to know this. they cured hepatitis c? sure. but did they fix the system that made you sick in the first place? 🤔
On October 25, 2025 AT 01:00
Abhi Yadav
life is pain bro 😔 the liver cries the heart bleeds same energy different vessel 🌀
On October 25, 2025 AT 02:56
Julia Jakob
so let me get this straight… you’re telling me my liver’s drama is secretly wrecking my heart? no wonder i’ve been feeling like a deflated balloon after 3 beers and a nap. i thought it was just aging. turns out i’ve got a silent roommate named HCV throwing wild parties in my arteries. thanks for the wake-up call… or whatever. 🤷♀️
On October 25, 2025 AT 19:49
Robert Altmannshofer
man, this is one of those posts that makes you stop scrolling. i used to think heart disease was just about burgers and sedentary jobs. turns out, your liver’s got a whole secret agenda. the part about DAAs cutting CRP by 30%? that’s huge. i’ve got a cousin who got cured last year-she started walking daily, swapped soda for sparkling water, and now her doc says her numbers look like a 30-year-old’s. it’s not magic. it’s science + choices. don’t wait for symptoms. get tested. your heart doesn’t text back when it’s in trouble.
On October 26, 2025 AT 20:58
Kathleen Koopman
so if you cure HCV… does your heart get a do-over? 🤔💖
On October 27, 2025 AT 06:44
Nancy M
the global burden of hepatitis C is staggering, yet public health messaging remains disproportionately focused on hepatic outcomes. cardiovascular implications are systematically underemphasized in primary care protocols, despite robust epidemiological data suggesting a causal pathway mediated by systemic inflammation. i urge clinicians to integrate cardiovascular risk stratification into routine HCV management frameworks. the data is unequivocal. the time for action is now.
On October 28, 2025 AT 17:24
gladys morante
they cured it but they didn’t cure the fact that you’re still a mess inside. now you’ve got a scarred liver and a heart that remembers the war. what’s the point of being virus-free if your body still feels like a war zone?
On October 29, 2025 AT 06:59
Precious Angel
let me be the first to say this: the pharmaceutical industry doesn’t want you to know that hepatitis C was never the real enemy. it was the lipid panels, the statin profits, the heart disease industrial complex. they gave you a 95% cure rate? sure. but did they tell you that your cholesterol was always a lie? that your heart was never broken by the virus-it was broken by the system that sold you fear, then sold you pills to fix it? you think you’re healed? you’re just another customer with a new prescription. 🤡
On October 29, 2025 AT 07:47
Melania Dellavega
i’ve been living with HCV for 12 years. never knew it was hurting my heart until i read this. i started eating more greens, walking after dinner, and got my first lipid panel in 5 years. turns out my HDL was trash. i’m on DAAs now. it’s not just about surviving. it’s about learning to live again-gently, intentionally. if you’re reading this and you’ve never been tested… please. your heart doesn’t scream. it just stops. don’t wait for silence.
On October 30, 2025 AT 08:00
Bethany Hosier
while the data presented is statistically compelling, one must consider the potential for confounding variables such as socioeconomic status, access to healthcare, and comorbid psychiatric conditions-all of which are disproportionately prevalent in populations with chronic hepatitis C. the correlation between HCV and cardiovascular events may not be causal, but rather indicative of systemic neglect in marginalized communities. one must ask: are we treating the virus-or the inequality?
On October 30, 2025 AT 23:27