Every time you pick up a prescription, you’re holding a safety check that could prevent a life-threatening mistake. But most people never look closely enough. A pill labeled 500 mg might be meant for you - or it could be ten times too strong. That’s not a hypothetical risk. In the U.S., about 1.3 million medication errors happen every year, and nearly a quarter of them involve the wrong strength or dose. You don’t need to be a pharmacist to catch these mistakes. You just need to know where to look and what to check.
Where to Find Medication Strength on the Label
The strength of your medication is the amount of active drug in each dose. It’s not hidden. It’s right there next to the name of the medicine. Look for numbers followed by units like mg (milligrams), mcg (micrograms), or iu (international units). For example:
- AMOXICILLIN 500 MG - each capsule contains 500 milligrams of amoxicillin
- HYDROCORTISONE 1% CREAM - each gram of cream contains 10 milligrams of hydrocortisone
- INSULIN GLARGINE 100 UNITS/ML - every milliliter has 100 units of insulin
Pharmacies in the U.S. are required by federal law to show this clearly. CVS, Walgreens, and Rite Aid all place it right under or beside the drug name. Some use bold text. Others put it in parentheses. Don’t assume the format is the same everywhere - but do assume the information is there. If you can’t find it, ask the pharmacist. It’s your right to know.
What Quantity Means - And Why It Matters
Quantity isn’t about how much you take each day. It’s how much the pharmacy gave you in total. This is easy to mix up. A label might say:
- 30 TABLETS - you got 30 pills total
- 120 ML - you got 120 milliliters of liquid
- 30 GRAMS - you got 30 grams of ointment
Don’t confuse this with your daily dose. If your doctor prescribed you to take one 500 mg pill twice a day, and you got 30 tablets, that’s a 15-day supply. If you only need 10 pills for the next two weeks, but you got 60, something’s off. That’s not always a mistake - maybe your doctor planned for a refill - but it’s worth checking.
Reading Liquid Medications: Concentration Is Key
Liquid medicines are where mistakes get dangerous. You’re not just reading a number - you’re reading a ratio. Look for something like 5 MG/5 ML. That means every 5 milliliters (about one teaspoon) contains 5 milligrams of the drug. If the label says 10 MG/5 ML, that’s twice as strong. Giving a child the wrong liquid dose can be deadly. A 2022 study by the American Society of Health-System Pharmacists found that over 32% of medication errors involving children happened because caregivers misread concentration ratios.
Here’s how to avoid it:
- Write down the concentration: 5 mg per 5 mL
- Know your child’s or patient’s prescribed dose: say, 2.5 mg
- Calculate: 2.5 mg is half of 5 mg, so you need half of 5 mL - that’s 2.5 mL
- Use the syringe or measuring cup that came with the medicine - never a kitchen spoon
If the label doesn’t show the concentration clearly, ask the pharmacist to explain it. Don’t guess.

Common Mistakes People Make - And How to Avoid Them
Even when the label is clear, people still misread it. Here are the top errors:
- Misreading decimal points: 0.25 mg looks like 25 mg if you glance too fast. That’s a 100-fold difference. Always pause. Read it slowly. Say it out loud: “zero point two five milligrams.”
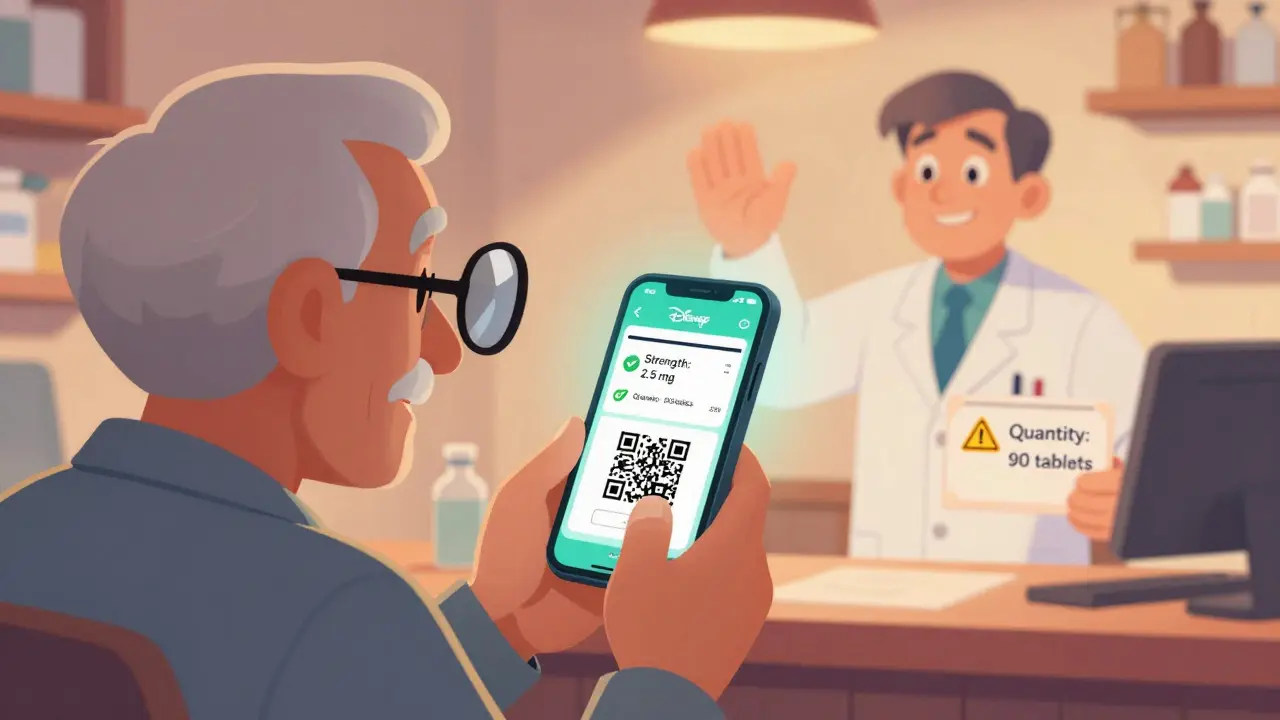
- Confusing total quantity with daily dose: You see “90 tablets” and think, “That’s a lot!” But if you take one a day, that’s three months’ supply. Don’t panic - just check your prescription.
- Missing units: mg vs. mcg is a 1,000x difference. If your blood pressure pill is supposed to be 2.5 mg and you get 2.5 mcg, it won’t work. If you get 25 mg instead, you could pass out.
- Ignoring the prescription number: Every label has an Rx#. Match it to the number your doctor gave you. If it doesn’t match, call the pharmacy.
A 2023 survey found that 63% of patients said the font on labels was too small. If you struggle to read it, ask for a large-print label. Most chain pharmacies offer this for free. You can also use your phone’s magnifier app - just point the camera at the label and zoom in.
Why This Checks Out: Real Stories, Real Safety
People who check their labels save lives - sometimes their own.
One Reddit user, u/MedSafetyMom, caught that her son’s amoxicillin was labeled 500 mg/5 mL instead of the prescribed 250 mg/5 mL. She called the pharmacy before giving him the first dose. They’d filled it with the adult strength. She saved him from a dangerous overdose.
Another patient in the Mayo Clinic forum shared that her blood pressure pill was filled as 10 mg instead of 2.5 mg. The pills looked different - but she didn’t know why. She only realized the error because she checked the label and compared it to her old prescription. She called her doctor, who confirmed the mistake.
These aren’t rare. The Patient Safety Network found that 22% of reported medication errors involved strength mismatches. Elderly patients are at highest risk - nearly 38% of cases involve people over 65. That’s why checking your label isn’t just good advice - it’s essential.
What’s Changing: New Tools and Regulations
The system is getting better. Since 2023, the FDA has required clearer labeling for high-risk drugs - especially those with narrow therapeutic windows, like blood thinners or seizure meds. By 2025, these labels will have stronger visual cues.
Many pharmacies now include QR codes on labels. Scan one with your phone, and you’ll get a link to the official FDA Medication Guide - with clear dosage instructions and warnings. CVS, Walgreens, and Kaiser Permanente have rolled this out widely.
Some stores are testing NFC tags - tap your phone on the label and get a voice reading of the strength and dosage. Early trials showed 89% of users felt more confident using them.
But tech won’t replace your eyes. Even with smart labels, the final safety check still falls to you. The FDA and Joint Commission both say: “The patient is the last line of defense.”
Your 4-Step Verification Checklist
Before you leave the pharmacy - or before you take any pill - run through this quick check:
- Find the drug name and strength - Look right beside the name. Is it in mg, mcg, or IU? Does it match what your doctor told you?
- Check the units - Is it 0.5 mg or 5 mg? 250 mcg or 250 mg? A single decimal point can kill.
- For liquids, confirm the concentration - Is it 5 mg per 5 mL? Or 5 mg per 1 mL? That’s a 5x difference. Know it before you measure.
- Match the quantity to your needs - Did you get enough for the full course? Too much? Call the pharmacy if it doesn’t line up.
Do this every time. Even if it’s the same medicine you’ve taken before. Pharmacies make mistakes. Pills change. Strengths change. Don’t assume.
When to Call the Pharmacy
You don’t need to be an expert to question a label. If anything feels off - call. Here are red flags:
- The pill looks different - color, shape, imprint
- The strength doesn’t match your previous prescription
- The quantity seems way too high or too low
- The label has handwriting on it - especially for strength
- You can’t read the numbers clearly
Pharmacists expect these calls. In fact, they’re trained to welcome them. A 2023 survey found that 76% of pharmacists said patients who asked questions prevented errors. You’re not being difficult. You’re being smart.
Final Thought: You’re the Final Safety Net
No system is perfect. Even with AI, barcode scans, and digital records, mistakes happen. But here’s the good news: you don’t need to fix the system. You just need to check the label.
It takes 30 seconds. It takes no money. It takes no special training. Just attention.
Medication errors kill thousands every year. Most of them are preventable. You holding that bottle in your hand? That’s the moment it stops being someone else’s problem - and becomes yours to fix.
Don’t just take it. Check it.
How do I know if the strength on my prescription label is correct?
Compare the strength listed on the label (like 500 mg or 2.5 mg) with the strength your doctor wrote on the prescription. If you’re unsure, call your doctor’s office or the pharmacy. Never assume - even if you’ve taken the same medicine before. Strengths can change, and pharmacies sometimes fill the wrong version.
What’s the difference between strength and quantity on a prescription label?
Strength tells you how much active drug is in each dose - for example, 10 mg per tablet. Quantity tells you how many doses you received - like 30 tablets or 120 mL of liquid. You might get 30 tablets of 10 mg each, meaning your total dose is 300 mg, but your daily dose is only 10 mg. Confusing these two is a common mistake.
Why is it dangerous to misread liquid medication concentrations?
Liquid medications list concentration as a ratio, like 5 mg per 5 mL. If you mistake it for 5 mg per 1 mL, you’re giving five times the intended dose. This is especially dangerous for children and elderly patients. A 2022 study found that over one-third of pediatric medication errors involved misreading concentration ratios. Always measure with the tool provided - never a kitchen spoon.
Can I trust the pharmacy to get the right strength?
Pharmacies follow strict rules, but humans still make mistakes. Studies show that 8.7% more errors occur in independent pharmacies than in big chains. Even at top pharmacies, 1 in 5 strength errors go unnoticed by staff. That’s why the FDA and Joint Commission call patients the “last line of defense.” Always double-check the label - even if you’ve been to that pharmacy for years.
What should I do if the label looks wrong?
Don’t take the medicine. Call the pharmacy immediately. Ask them to verify the prescription against the original order. If they dismiss your concern, call your doctor. You have the right to safe medication. If you suspect an error, report it to the pharmacy’s customer service and ask for a written explanation. Most pharmacies have error-reporting systems in place - and they’re required to investigate.
