Many people don’t realize that their everyday painkillers could be quietly damaging their liver. If you’re taking a prescription pain medication like Vicodin, Percocet, or any other combo pill, you’re likely getting acetaminophen - the same active ingredient in Tylenol. The problem? You might be taking it from multiple sources at once and not even know it.
Why Acetaminophen Combination Products Are Risky
Acetaminophen is safe when used correctly. But when it’s mixed with opioids like hydrocodone or oxycodone, it becomes a hidden danger. These combination products are common: doctors prescribe them for moderate to severe pain after surgery, injury, or chronic conditions. But patients often don’t realize that every tablet contains acetaminophen - sometimes 325 mg per pill. That’s the maximum amount allowed per dose since the FDA’s 2014 rule change.Here’s the catch: if you’re also taking Advil PM, NyQuil, Excedrin, or even a generic cold medicine, you could be adding more acetaminophen without thinking. The total daily limit for adults is 4,000 mg. But if you take three Vicodin tablets (325 mg each) and two extra-strength Tylenol (500 mg each), you’ve already hit 2,000 mg - and you’re not even halfway through the day.
In the U.S., acetaminophen overdose is the top cause of acute liver failure. About 40% of those cases come from unintentional overdoses involving combination products. Even worse, a 2019 study found that nearly 7 out of 10 of these overdoses weren’t deliberate - people just didn’t know they were doubling up.
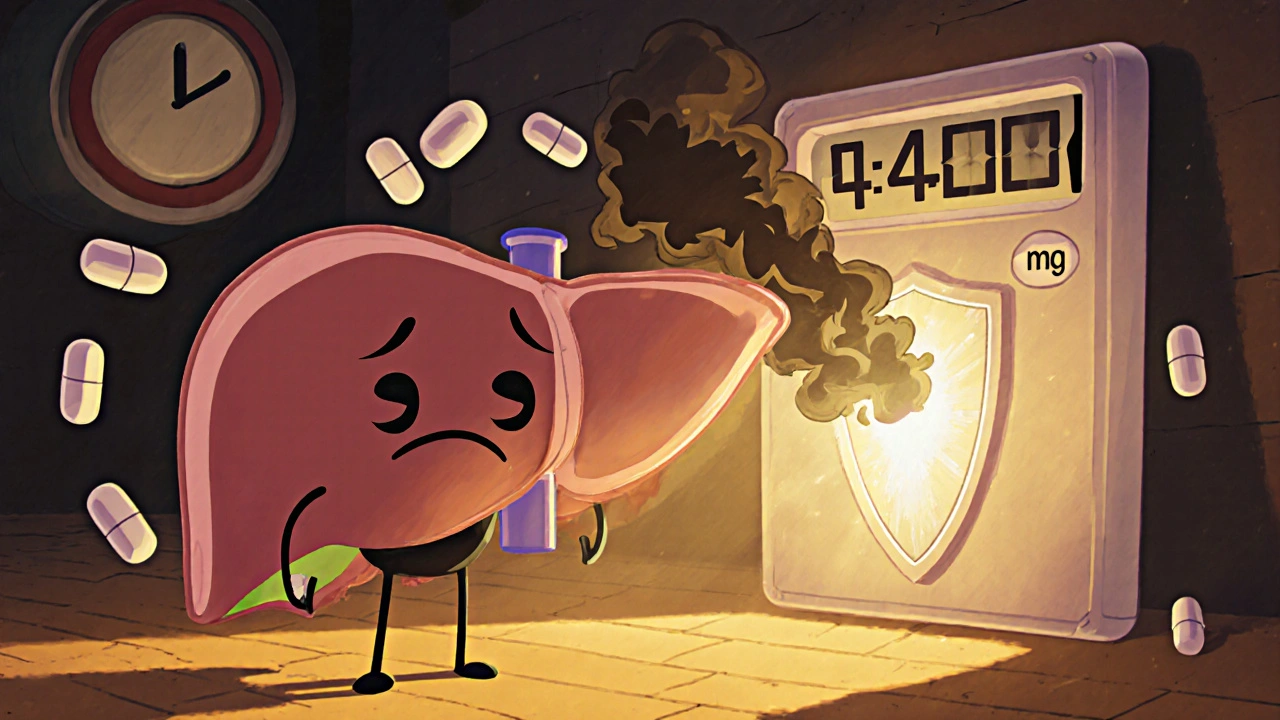
How Your Liver Gets Hurt
Your liver breaks down acetaminophen using two main pathways: glucuronidation and sulfation. These are safe at normal doses. But when you take too much, those pathways get overwhelmed. The liver starts converting acetaminophen into a toxic byproduct called NAPQI.Normally, your body neutralizes NAPQI with glutathione - a natural antioxidant. But when you overload your system, glutathione runs out. Without it, NAPQI starts attacking liver cells, damaging mitochondria and triggering inflammation. This can lead to cell death, liver failure, or even death if not caught early.
Studies show that liver damage becomes likely when glutathione drops below 30% of normal levels. That can happen after just a few extra pills over a couple of days. People with alcohol use disorder, poor nutrition, or existing liver disease are at higher risk because their glutathione stores are already low.
What You Can Do to Stay Safe
The good news? Almost all acetaminophen-related liver injuries are preventable. Here’s how:- Read every label - even the small print. Look for “acetaminophen,” “APAP,” or “paracetamol” on all medicines. It’s in more than 600 OTC and prescription products. If you see it on more than one, stop and count the total.
- Know your daily limit. The max is 4,000 mg for healthy adults. But if you drink alcohol regularly, have liver disease, or are underweight, cut that to 2,000-3,000 mg. Many doctors now recommend 2,000 mg as the default for safety.
- Never mix prescription and OTC painkillers without checking. If your doctor gives you a combo pill, ask: “Is there acetaminophen in this?” Then check your medicine cabinet for anything else with it.
- Use a medication tracker. Write down every pill you take, including doses and times. Apps like MyTherapy or the new NIH-backed barcode scanner tool (currently in beta) can auto-detect acetaminophen in 150+ products by scanning the barcode.
- Ask your pharmacist. Pharmacists are trained to spot dangerous overlaps. In one 2021 study, pharmacist-led counseling reduced unintentional overdoses by 41%. Don’t be shy - bring all your meds in for a quick review.
What Doctors and Pharmacists Should Be Doing
Healthcare providers play a huge role. The CDC now requires electronic health records (like Epic) to track cumulative acetaminophen doses across all prescriptions. If your doctor prescribes hydrocodone/acetaminophen and you already have a prescription for oxycodone/acetaminophen, the system should flag it.But training matters. A 2022 Johns Hopkins study found that only 62% of patients understood their acetaminophen risk after a standard doctor visit - even after being told. Doctors need at least three hours of special training to explain this clearly. Many still don’t get it.
Pharmacists are stepping up. In the EU, mandatory counseling for combo products led to a 31% drop in hospitalizations. In the U.S., multilingual medication guides (available in 14 languages) help non-English speakers - who are 2.3 times more likely to overdose.
What’s New in Treatment and Prevention
If someone does overdose, time is critical. The standard antidote is N-acetylcysteine (NAC), which replenishes glutathione and protects liver cells. It works best if given within 8 hours - but studies show it still helps up to 48 hours after ingestion.Now there’s a new option: fomepizole. Approved by the FDA in 2021, it blocks the enzyme that turns acetaminophen into NAPQI. One 2022 study showed it cut severe liver injury by 32% when used with NAC.
There’s also a new extended-release NAC tablet that lasts 12 hours instead of 4. That’s a game-changer - many people stop taking NAC early because the old version requires 21 doses over 72 hours. Now, compliance is improving.
Researchers are also testing natural compounds like emodin (from rhubarb) and sulforaphane (from broccoli sprouts). These activate the body’s own antioxidant defenses and have shown promise in animal studies. But experts warn: don’t rely on supplements. They’re not substitutes for safe dosing.
Real Stories, Real Risks
On Reddit, a 2022 thread asking “How many people know their painkiller has acetaminophen?” got over 1,200 replies. Two-thirds admitted they’d accidentally taken too much before.One woman in Ohio took Vicodin for a back injury and NyQuil for a cold. She didn’t realize both had acetaminophen. After two weeks, her liver enzymes spiked. She spent five days in the hospital. “I thought I was being careful,” she wrote. “I didn’t even know Tylenol was in the Vicodin.”
On the flip side, one Amazon review from March 2023 praised the new red warning labels on Vicodin boxes: “It made me check everything else I was taking. I almost took Advil PM with it - now I know better.”

Why This Isn’t Just a U.S. Problem
The FDA’s 2014 limit of 325 mg per dose in prescription combos was mirrored by the European Medicines Agency in 2013. In the UK, the MHRA advises a maximum of 4,000 mg per day - same as the U.S. But compliance varies.Since 2017, EU countries require pharmacists to counsel patients on acetaminophen risks before dispensing combo products. That’s helped reduce hospitalizations by 31%. In the U.S., the “Know Your Dose” campaign has reached 89 million people since 2012, but awareness still lags.
And here’s something surprising: prescriptions for opioid/acetaminophen combos have dropped 43% since 2010 - not just because of the opioid crisis, but because more people are now aware of the liver risks.
What’s Next?
The FDA is now considering lowering the maximum dose in OTC acetaminophen products from 1,000 mg per tablet to 650 mg. That could reduce accidental overdoses even further.Meanwhile, lawsuits are piling up. Over 1,200 legal cases since 2010 have resulted in $1.2 billion in settlements. Manufacturers are being held accountable for unclear labeling and insufficient warnings.
But the biggest challenge remains: polypharmacy and low health literacy. People take multiple meds. They don’t read labels. They assume “natural” or “prescription” means safe. That mindset kills.
The solution isn’t just better pills or new drugs. It’s better education - for patients, for doctors, for pharmacists. It’s about making the invisible visible. Acetaminophen isn’t dangerous because it’s toxic. It’s dangerous because we forget it’s there.
Can I take acetaminophen if I drink alcohol?
If you drink alcohol regularly - even just a few drinks a week - your liver’s ability to process acetaminophen is reduced. Experts recommend limiting acetaminophen to 2,000 mg per day at most, and avoiding it entirely if you binge drink or have liver disease. Never take acetaminophen while intoxicated.
Is it safe to take acetaminophen every day for chronic pain?
Long-term daily use of acetaminophen, even at 3,000 mg, can slowly damage the liver over time. If you need daily pain relief, talk to your doctor about alternatives like physical therapy, NSAIDs (if appropriate), or non-drug treatments. Don’t assume acetaminophen is harmless just because it’s available over the counter.
What should I do if I think I’ve taken too much acetaminophen?
Call Poison Control immediately at 1-800-222-1222 (U.S.) or go to the nearest emergency room. Do not wait for symptoms. Liver damage can happen without nausea or pain in the early stages. The sooner you get treatment, the better your chances of recovery.
Are generic brands safer than name brands like Tylenol?
No. Generic acetaminophen has the same active ingredient and carries the same risks. The only difference is price. Always check the active ingredients list - not the brand name. A generic cold medicine can have just as much acetaminophen as Tylenol.
Do children’s acetaminophen products carry the same risks?
Children’s formulas are dosed by weight, not age, and are much less likely to cause overdose if used correctly. But accidental overdoses still happen - often when parents give multiple products or use the wrong measuring tool. Always use the dosing device that comes with the medicine, and never guess.
Can I use herbal supplements to protect my liver from acetaminophen?
Supplements like milk thistle or NAC pills are not proven to prevent liver injury from overdose. While research on compounds like sulforaphane is promising, they’re not substitutes for accurate dosing. Relying on supplements can give a false sense of safety. Stick to the facts: know your dose, read labels, and avoid mixing meds.

Comments
Robert Altmannshofer
Man, I had no idea my cold medicine had acetaminophen in it. Took NyQuil for a week after surgery and didn't think twice. Glad I read this before I ended up in the ER. Now I check every label like it's a treasure map. 🗺️
On November 22, 2025 AT 23:09
Kathleen Koopman
OMG I just checked my cabinet and found 4 different things with APAP 😱 I’m deleting my meds app and starting over. This is wild how sneaky it is.
On November 23, 2025 AT 17:10
Nancy M
It’s staggering how many people assume ‘prescription’ means ‘safe’ - especially when the label doesn’t scream danger. The FDA’s 2014 limit was a step forward, but education needs to be as ubiquitous as the drug itself. We’re treating symptoms, not the root cause: complacency.
On November 25, 2025 AT 16:04
gladys morante
Everyone’s acting like this is some new revelation. I’ve been telling people for years that Tylenol is a silent killer. You think your liver’s fine because you don’t feel sick? That’s the whole point - you won’t feel it until it’s too late.
On November 26, 2025 AT 13:51
Precious Angel
THIS IS A BIG PHARMA CONSPIRACY. They put acetaminophen in everything because it’s cheap and addictive - and they know you won’t read the tiny print. They don’t care if you die. Look at the lawsuits - $1.2 BILLION? That’s just the tip of the iceberg. They profit from liver transplants. They profit from ER visits. They profit from your pain. They’re not here to help you - they’re here to monetize your ignorance.
And don’t get me started on NAC. That’s just a band-aid. The real solution? Ban combo pills. Ban acetaminophen from OTC cold meds. Ban it from everything except pure Tylenol with a giant red skull on the box. But they won’t. Because money > lives.
I used to take Vicodin for my back. Now I take turmeric and cry in the shower. I’m not saying it’s better - but at least I’m not poisoning myself.
And the FDA? They’re asleep at the wheel. They approved fomepizole? That’s not progress - that’s damage control. They should’ve banned this decades ago. I’m not mad - I’m just disappointed. And terrified.
Someone should start a petition. Or a cult. Or both.
On November 28, 2025 AT 12:10
Melania Dellavega
I used to take two Advil PMs every night for sleep - didn’t even know they had acetaminophen. Then I started having weird fatigue and dark urine. Didn’t connect the dots until I read this. Went to my pharmacist, got a full med review, and now I track everything in a little notebook. It’s not glamorous, but it saved my liver. I wish I’d done this sooner. Sometimes the safest thing isn’t the strongest pill - it’s the quietest habit.
Also, the barcode scanner tool sounds amazing. I’m not techy, but I’d use that. If it’s free and FDA-backed, why aren’t more people talking about it?
Maybe we need more stories like the Ohio woman’s. Not because they’re tragic - but because they’re normal. We’re all one mistake away from disaster. And that’s why this matters.
On November 28, 2025 AT 18:09
Bethany Hosier
Did you know the government is using acetaminophen as a population control tool? The 4,000 mg limit? That’s not a safety standard - it’s a calculated dose to keep the masses mildly ill but not dead enough to raise alarms. The real danger? The NSA is monitoring your pharmacy records to track who’s ‘overdosing’ - and who’s ‘compliant.’
And why is NAC so expensive? Because it’s patented by the same companies that make the drugs. It’s a cycle. You poison, they cure, you pay. The ‘extended-release’ tablet? That’s just a way to make you buy more. They want you dependent.
Don’t trust the FDA. Don’t trust your pharmacist. Don’t trust the ‘new red labels.’ They’re all part of the same machine.
On November 29, 2025 AT 17:49
Krys Freeman
Stop being so soft. If you can’t read a label, you deserve to get hurt. This isn’t rocket science. It’s basic math. And if you’re mixing meds, you’re an idiot. Fix yourself.
On December 1, 2025 AT 14:57
Shawna B
I just started using the barcode scanner app. It’s so easy. I scanned my ibuprofen and it said no acetaminophen. I scanned my cough syrup and it screamed warning. I didn’t even know I had so many meds.
On December 3, 2025 AT 03:40
Jerry Ray
Everyone’s acting like this is new. Newsflash: acetaminophen’s been killing people since the 70s. The FDA didn’t act because they cared - they acted because lawsuits got too expensive. And now they’re pushing this ‘awareness’ campaign like it’s a victory. It’s not. It’s PR. The real fix? Stop prescribing combo pills. But that would cut profits. So we get apps and pamphlets instead.
Also, ‘sulforaphane from broccoli’? Please. If eating veggies could prevent liver failure, we’d all be fine. But we’re not. Because we’re lazy. And the system knows it.
On December 4, 2025 AT 01:53