When we talk about Vascular disease is a group of disorders that affect arteries, veins, and capillaries, often leading to reduced blood flow, clot formation, or vessel damage, the first step is to know what puts you at risk. This guide breaks down the most common contributors, how they work together, and what you can do right now to protect your vessels.
Understanding Vascular Disease
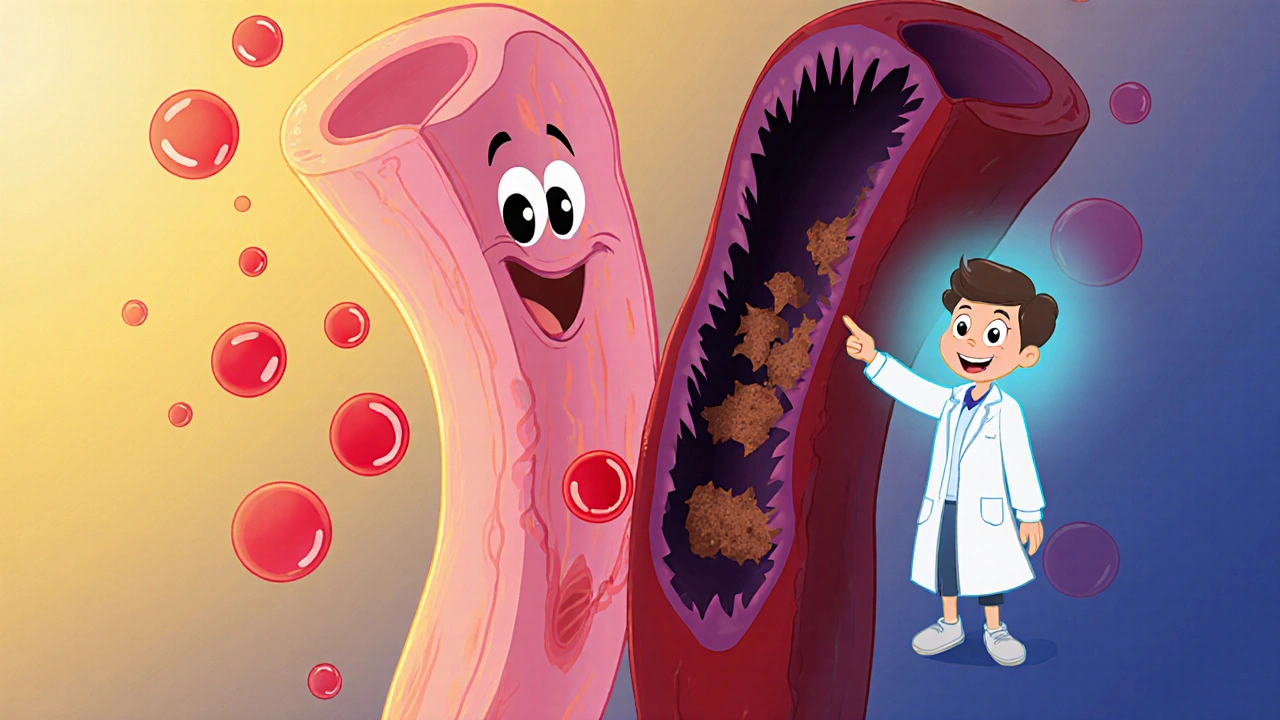
Vascular disease isn’t a single condition; it covers everything from atherosclerosis and peripheral artery disease to aneurysms. The common thread is that the blood vessels can’t perform their job of delivering oxygen‑rich blood efficiently. When vessels narrow or harden, the heart works harder, and organs may suffer from chronic low‑grade ischemia.
Non‑Modifiable Risk Factors
Some risk factors are baked into your DNA or life timeline. You can’t change them, but you can plan around them.
- Age is a powerful predictor; after 45 for men and 55 for women, the chance of developing atherosclerotic plaques climbs sharply.
- Family history of heart attack, stroke, or peripheral artery disease doubles your baseline risk.
- Sex matters-men tend to develop coronary artery disease earlier, while women’s risk spikes after menopause.
Knowing these facts helps you ask the right questions during a health check and motivates early screening.
Modifiable Risk Factors
These are the levers you can pull to lower your odds dramatically.
- Hypertension high blood pressure forces vessel walls to stretch, fostering micro‑tears that become entry points for plaque.
- High cholesterol elevated LDL levels deposit fatty material on arterial walls, creating the classic “yellow streaks” of atherosclerosis.
- Smoking tobacco use damages the endothelium, reduces nitric oxide, and accelerates plaque buildup.
- Diabetes high blood sugar glycosylates proteins in vessels, making them stiff and prone to clot formation.
- Obesity excess body fat raises inflammatory markers and often co‑exists with hypertension and dyslipidaemia.
- Physical inactivity sedentary lifestyle deprives muscles of the benefits of regular blood flow, worsening insulin resistance and lipid profiles.
Each factor can be measured, tracked, and improved with evidence‑based steps.

How Risk Factors Interact
Think of risk factors as ingredients in a recipe. When you combine hypertension with high cholesterol, the chance of a plaque rupturing and causing a stroke can be more than double the risk of either factor alone. This synergistic effect is why doctors use risk calculators that weight each variable.
For example, the QRISK3 algorithm (used in the UK) assigns points for age, ethnicity, smoking status, blood pressure, cholesterol ratios, and more. A 55‑year‑old male smoker with a systolic pressure of 150 mmHg and LDL of 4.0 mmol/L scores around 15% 10‑year risk of a major vascular event-significantly higher than any single factor would suggest.
Assessing Your Personal Risk
Start with a simple checklist, then move to a formal risk calculator.
- Gather your latest numbers: blood pressure, fasting glucose, lipid panel, weight, and waist circumference.
- Note lifestyle habits: cigarettes per day, weekly exercise minutes, diet quality.
- Enter the data into a reputable tool like QRISK3, ASCVD Risk Estimator, or the European SCORE system.
- Discuss the output with your GP or cardiologist-your risk score guides treatment intensity.
Even if you’re not in the high‑risk bracket, the exercise of measuring these numbers often uncovers hidden problems early.
Prevention Strategies that Work
Here’s a quick‑hit action plan that addresses the biggest vascular disease risk factors you can control.
- Blood pressure control: Aim for < 130/80 mmHg. Lifestyle tweaks (lower salt, DASH diet) and, when needed, ACE inhibitors or ARBs are first‑line.
- Cholesterol management: Target LDL < 2.0 mmol/L for high‑risk patients. Statins are proven to cut major events by ~25% per 1 mmol/L LDL reduction.
- Smoking cessation: Use nicotine replacement, varenicline, or behavioral counseling. Quitting < 12 months reduces heart attack risk by ~50%.
- Diabetes control: Keep HbA1c below 7% (or individualized target). Metformin plus GLP‑1 agonists have favorable vascular profiles.
- Weight loss: Losing 5‑10% of body weight improves blood pressure, triglycerides, and insulin sensitivity.
- Physical activity: At least 150 minutes of moderate‑intensity aerobic exercise weekly (e.g., brisk walking, cycling).
- Dietary overhaul: Embrace a Mediterranean or plant‑forward diet-rich in fruits, veg, whole grains, nuts, and olive oil.
Small, consistent changes beat drastic crash diets. Track progress with a health app or a simple journal.

When to Seek Medical Help
If you notice any of these warning signs, call your GP or an emergency service immediately:
- Sudden chest pain or pressure lasting > 5 minutes.
- Unexplained shortness of breath, especially at rest.
- New weakness, numbness, or difficulty speaking (possible stroke).
- Pain in the calf or foot that worsens with walking (possible peripheral artery disease).
Early intervention can restore blood flow and prevent irreversible damage.
Quick Comparison of Major Modifiable Risk Factors
| Risk Factor | Category | Typical Measurement | Relative Risk Increase (if uncontrolled) |
|---|---|---|---|
| Hypertension | Blood pressure | Systolic > 140 mmHg | ~2‑3× for stroke, 1.5‑2× for coronary events |
| High cholesterol | Lipid profile | LDL > 3.0 mmol/L | ~2× for heart attack |
| Smoking | Lifestyle | ≥ 10 cigarettes/day | ~2‑4× for peripheral artery disease |
| Diabetes | Metabolic | HbA1c > 6.5% | ~1.8‑2.5× for atherosclerosis |
| Obesity | Body composition | BMI > 30 kg/m² | ~1.5‑2× for coronary disease |
| Physical inactivity | Activity level | < 30 min/week moderate activity | ~1.3‑1.5× for heart attack |
Take‑Away Checklist
- Know your numbers: blood pressure, cholesterol, glucose, weight.
- Quit smoking - even cutting back yields immediate vascular benefits.
- Adopt a heart‑healthy diet and aim for at least 150 min of moderate exercise weekly.
- Schedule an annual risk assessment with your GP, especially if you’re over 45 or have a family history.
- Act quickly on any new chest, leg, or neurological symptoms.
What is the difference between atherosclerosis and peripheral artery disease?
Atherosclerosis refers to plaque buildup inside any artery, most commonly the coronary or carotid arteries. Peripheral artery disease (PAD) is a specific manifestation of atherosclerosis that narrows arteries in the legs, causing pain during walking (claudication) and increasing ulcer risk.
Can women develop vascular disease without traditional risk factors?
Yes. Hormonal changes, especially post‑menopause, can raise LDL and lower HDL even in the absence of high blood pressure or smoking. Women also more often present with microvascular disease, which affects small vessels and may not show up on standard imaging.
How often should I have my cholesterol checked?
If you have no risk factors, every 5 years is usually fine. With hypertension, diabetes, or a family history, an annual lipid panel is recommended.
Is a low‑carb diet better for preventing vascular disease?
Evidence shows that diets rich in whole grains, fruits, and unsaturated fats (Mediterranean style) consistently lower LDL and blood pressure. Low‑carb diets can work if they limit saturated fats and include plenty of veg, but the overall evidence favours a balanced Mediterranean approach.
What first‑line medication is usually prescribed for high blood pressure?
Guidelines recommend ACE inhibitors or ARBs as initial therapy for most adults, especially if they have diabetes or chronic kidney disease. Calcium‑channel blockers and thiazide diuretics are also common choices.
Comments
Krys Freeman
This guide is textbook BS. Everyone knows if you eat bacon and don't run marathons, you're gonna die. No need for all this fluff.
On October 24, 2025 AT 11:32
Shawna B
So high blood pressure and smoking are bad yeah but what about sugar
On October 24, 2025 AT 13:42
Jerry Ray
Actually the real cause of vascular disease is government-mandated vegetable oils and fake butter. They replaced real fat with trans fats in the 70s and now everyone's dropping dead from clogged arteries. The lipid hypothesis is a scam.
On October 24, 2025 AT 16:11
David Ross
Let me be perfectly clear: hypertension, hyperlipidemia, and tobacco use are the primary, evidence-based, modifiable risk factors for atherosclerotic cardiovascular disease-period. The data is irrefutable. If you're ignoring this, you're not just uninformed-you're endangering yourself and others.
On October 26, 2025 AT 03:51
Sophia Lyateva
theyre hiding the truth about vascular disease its not cholesterol its the fluoride in the water and the 5g towers making your arteries vibrate wrong
On October 26, 2025 AT 13:47
AARON HERNANDEZ ZAVALA
I get what the article is saying and I think it's helpful but I also think we need to talk about stress and sleep more. I know people who eat perfect and exercise but work 80 hours a week and still have heart issues. It's not just numbers.
On October 27, 2025 AT 04:55
Lyn James
Let’s be honest-this whole society is a walking time bomb. We’ve been sold a lie that convenience is worth more than longevity. We microwave our meals, sit in chairs all day, and then wonder why our arteries are clogged like a sink full of grease. We’ve replaced wisdom with Wi-Fi and discipline with dopamine. The real problem isn’t cholesterol-it’s the moral decay of a culture that treats the body like a disposable machine. If you don’t respect your vessel, your vessel won’t respect you. And don’t even get me started on how we’ve normalized obesity as ‘body positivity’ while ignoring the silent erosion of our circulatory systems.
On October 27, 2025 AT 07:39
Craig Ballantyne
The QRISK3 algorithm is robust, but its validation in non-UK populations remains limited. While the modifiable risk factors outlined are well-established, the clinical utility of absolute risk stratification depends heavily on local epidemiology and access to pharmacotherapy. In resource-limited settings, population-level interventions-salt reduction, smoking cessation campaigns-are more scalable than individualized lipid targets.
On October 27, 2025 AT 11:37