When you hear the word statin, most doctors think of a lifesaver. For millions of people, these pills have stopped heart attacks before they happen. But for others, the same pills bring aching legs, tired muscles, and sleepless nights wondering if the benefit is worth the cost. The truth isn’t black and white. Statins work - powerfully - but they aren’t harmless. Understanding both sides lets you make a smarter choice.
How Statins Actually Lower Cholesterol
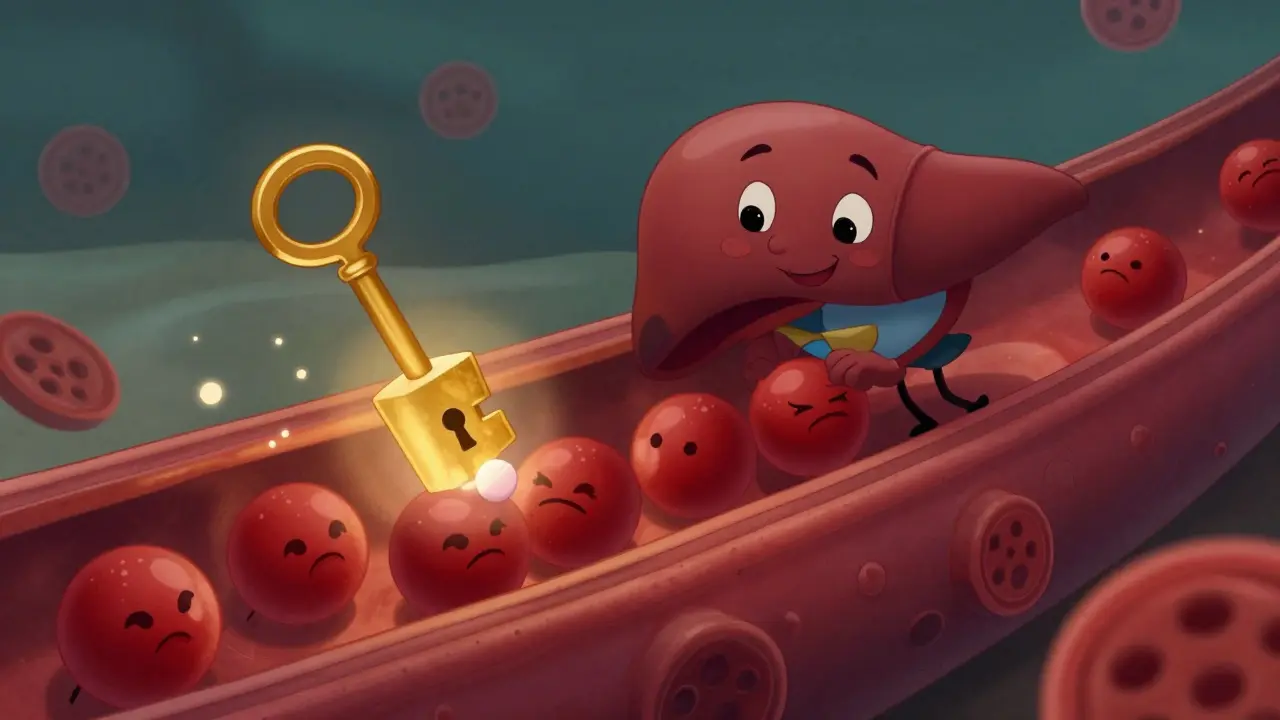
Statins don’t just block cholesterol. They rewire how your liver works. Your body makes about 75% of its cholesterol naturally, mostly in the liver. The key enzyme responsible? HMG-CoA reductase. Statins latch onto this enzyme like a key jammed in a lock, stopping it from doing its job. That forces your liver to pull more LDL - the "bad" cholesterol - out of your blood to make up for the shortage.
The result? LDL drops by 30% to 60%, depending on the drug and dose. Atorvastatin at 40 mg can knock LDL down by over 50%. Rosuvastatin at 20 mg does the same. That’s not a small change. For every 1 mmol/L (39 mg/dL) drop in LDL, your risk of a heart attack or stroke falls by about 22%. That’s backed by decades of studies - from the 4S trial in the 90s to modern data from over 200,000 patients.
It’s not just about cholesterol numbers. Statins also calm inflammation inside artery walls. They stabilize plaque so it’s less likely to rupture and cause a clot. They help the lining of your blood vessels relax and work better. These effects kick in fast - sometimes within weeks - even before LDL drops significantly. That’s why some people feel better before their lab results change.
The Real Risk: Muscle Pain Isn’t Rare
If you’ve been on a statin and noticed sore thighs, stiff shoulders, or cramps in your calves after walking, you’re not imagining it. Muscle pain is the most common side effect. Studies show between 5% and 29% of people report it. That’s not a tiny number. It’s more common than most doctors admit.
Most cases are mild - a dull ache, not a sharp pain. But for some, it’s bad enough to stop daily life. One man on Reddit described leg cramps so severe he could barely walk. Another said his shoulders felt like they were full of sand. These aren’t outliers. They’re real people. And many stop taking their statins because of it.
The scary part? Only about 0.1% of users develop rhabdomyolysis - a rare, dangerous breakdown of muscle tissue that can damage kidneys. But the much more common problem is myalgia: muscle pain without any lab abnormalities. Doctors often dismiss it as "just aging" or "not serious." But if it’s making you skip walks, avoid stairs, or wake up stiff, it’s serious to you.
Why Do Statins Hurt Muscles?
It’s not fully understood, but science has clues. Statins don’t just block cholesterol production. They also reduce levels of coenzyme Q10 (CoQ10), which your muscles need to make energy. Think of it like draining the battery in your car’s starter motor - the engine still runs, but it struggles. Some people have lower natural CoQ10 levels, and for them, statins can feel like a double hit.
Genetics play a role too. A gene called SLCO1B1 controls how your liver absorbs statins. If you have a certain variant, your body holds onto more of the drug, especially simvastatin. That raises the chance of muscle damage. It’s not tested routinely - but if you’ve had muscle pain on one statin and it cleared up after switching, that’s a sign your genes might be involved.
Age, kidney or liver issues, diabetes, thyroid problems, and taking other meds (like certain antibiotics or grapefruit juice) can also make muscle pain worse. It’s rarely one thing. It’s a mix.

What to Do If You Have Muscle Pain
Don’t quit cold turkey. Stopping statins increases your heart attack risk - fast. A JAMA study found nearly half of people stop within a year, and many end up in the ER with heart problems within months.
Instead, talk to your doctor. Here’s what works:
- Switch statins. Not all are the same. Pravastatin and fluvastatin are less likely to cause muscle pain. Rosuvastatin and atorvastatin are stronger but can be harder on muscles. Try switching from simvastatin to pravastatin - many people find relief.
- Lower the dose. Sometimes 10 mg of atorvastatin gives you 80% of the benefit with half the side effects. You don’t need the highest dose unless you’re at very high risk.
- Try every-other-day dosing. Some statins, like atorvastatin, last long enough in your body to work even if you take them every 48 hours. This cuts exposure and often eases pain.
- Check CoQ10. A small trial showed 100-200 mg of CoQ10 daily reduced muscle pain in half the users. It’s not a miracle, but it’s cheap and safe to try.
- Test your thyroid and vitamin D. Low levels of either can mimic statin pain. Fix those first.
And yes - get your creatine kinase (CK) tested if pain is severe. It’s a simple blood test. If CK is more than 5 times the upper limit, you may need to stop.
Who Should Be on Statins - and Who Shouldn’t
Statins aren’t for everyone. They’re strongest for people who:
- Already had a heart attack or stroke
- Have diabetes and are over 40
- Have very high LDL (190 mg/dL or more)
- Have a 10-year risk of heart disease over 7.5% (calculated by your doctor using age, blood pressure, cholesterol, smoking)
For others - especially healthy people with only mildly high cholesterol - the benefit is much smaller. A 60-year-old woman with LDL 140 and no other risks might lower her heart attack risk by less than 1% over 10 years. Is that worth muscle pain? Maybe not.
That’s why guidelines now stress shared decision-making. You should know your risk, know your options, and decide together with your doctor. No one-size-fits-all.

Real-World Numbers: What Patients Actually Experience
On Drugs.com, atorvastatin (Lipitor) has a 5.8 out of 10 rating from nearly 2,000 reviews. About 43% say it helped. 34% say it hurt. Simvastatin scores a bit higher at 6.2, but still, over a third report side effects.
On Reddit’s r/Statins, the stories are raw. One user switched from rosuvastatin to pravastatin and said, "I went from limping to hiking again in 3 weeks." Another said, "My doctor said my pain was "just stress." I quit. My cholesterol went up. My knees stopped hurting. I’m choosing quality of life."
These aren’t just complaints. They’re signals. Your body is talking. Listen.
The Bottom Line: Balance, Not Fear
Statins are among the most studied drugs in history. Their benefits for high-risk people are undeniable. They save lives. But they’re not perfect. Muscle pain is real, common, and often ignored.
You don’t have to choose between a heart attack and aching legs. There’s a middle ground. Try a different statin. Lower the dose. Add CoQ10. Check your thyroid. Test your genes if you can. Work with your doctor - not against them.
If you’re low risk, ask: "Do I really need this?" If you’re high risk and in pain, ask: "What’s the next best option?"
There’s no shame in needing help. There’s also no shame in saying, "This isn’t working for me." The goal isn’t to take a pill forever. It’s to live well - heart healthy, strong, and free of pain.
Do statins really prevent heart attacks?
Yes, for people at high risk. For every 1 mmol/L drop in LDL cholesterol, major heart events drop by about 22%. In people who’ve had a heart attack, statins cut the chance of another by nearly 40% over five years. The benefit is strongest when risk is highest.
Can muscle pain from statins go away on its own?
Sometimes, yes. Mild muscle aches often improve after a few weeks as your body adjusts. But if pain gets worse or lasts more than a month, it’s not normal. Don’t wait it out - talk to your doctor. Persistent pain can be a sign you need a different statin or dose.
Is it safe to stop statins if I have muscle pain?
Only under medical supervision. Stopping statins suddenly increases your risk of heart attack or stroke - especially in the first year. Many people who quit because of pain end up hospitalized later. Always work with your doctor to find a solution before stopping.
Are generic statins just as good as brand names?
Yes. Atorvastatin, simvastatin, and rosuvastatin generics work exactly like their brand-name versions. The only difference is cost. Generic atorvastatin can cost as little as $4 a month. You’re not sacrificing effectiveness - you’re saving money.
Can I take CoQ10 with statins?
Yes, and many doctors recommend it if you have muscle pain. CoQ10 helps muscles produce energy, and statins lower its levels. Studies show 100-200 mg daily can reduce pain in about half of users. It’s safe, inexpensive, and worth trying before switching drugs.
What’s the best statin for avoiding muscle pain?
Pravastatin and fluvastatin are generally the least likely to cause muscle issues. Rosuvastatin and simvastatin carry higher risk, especially at high doses. If you’ve had pain on one statin, switching to pravastatin often helps. Always discuss options with your doctor - your risk level matters too.
Should I get genetic testing for statin sensitivity?
Not routinely - but if you’ve had severe muscle pain on multiple statins, it’s worth considering. A variant in the SLCO1B1 gene increases the risk of simvastatin-induced myopathy. Testing isn’t standard, but it can explain why some people react badly while others don’t.
Do statins cause weight gain?
No direct link. Statins don’t cause weight gain. But some people feel less pain after switching to a better statin and become more active - which might lead to weight loss. Others feel tired and move less, which could lead to weight gain. It’s indirect. Focus on movement and diet, not the pill.
Next Steps: What to Do Today
If you’re on a statin and feel fine - keep taking it. You’re doing something important.
If you’re on a statin and feel pain - don’t ignore it. Write down when it happens, where it hurts, and how bad it is. Bring that list to your doctor. Ask: "Could this be the statin? What are my alternatives?"
If you’re not on a statin but have high cholesterol - ask your doctor to calculate your 10-year heart risk. If it’s under 5%, lifestyle changes might be enough. If it’s over 10%, statins could be worth it - even if you’re worried about side effects.
There’s no perfect drug. But there is a right choice for you - if you ask the right questions.