Why Your Sleep Position Matters More Than You Think
If you snore loudly, wake up gasping, or feel exhausted even after eight hours in bed, your sleep position might be the missing piece. For many people with obstructive sleep apnea (OSA), sleeping on their back isn’t just uncomfortable-it’s dangerous. The difference between lying on your back and sleeping on your side can mean the difference between 30 breathing pauses an hour and fewer than five. This isn’t speculation. It’s backed by sleep studies and clinical data from the American Academy of Family Physicians and the American Academy of Sleep Medicine.
What Happens When You Sleep on Your Back?
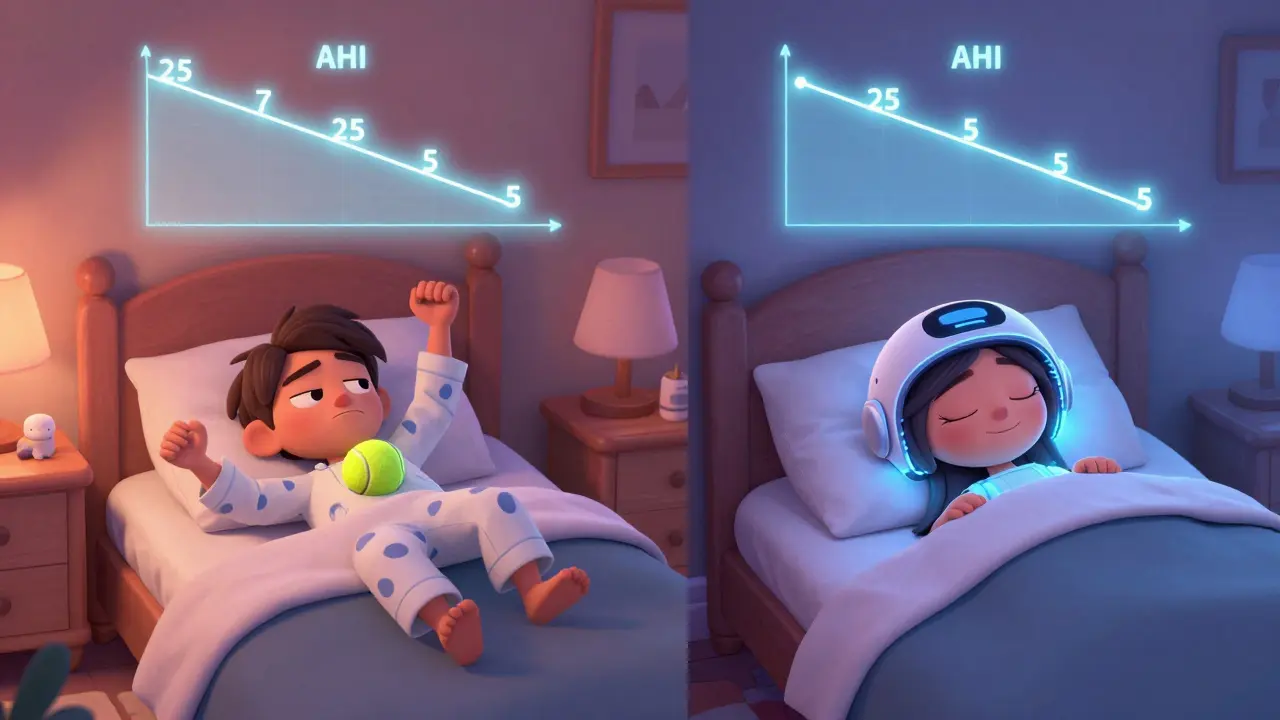
When you lie flat on your back, gravity pulls your tongue and soft tissues in your throat backward. This narrows your airway by 30-40%, making it easier for it to collapse during sleep. That’s when apnea events happen-moments when breathing stops for 10 seconds or longer. For people with positional obstructive sleep apnea (POSA), this only happens when they’re on their back. Their apnea-hypopnea index (AHI) can be more than double in the supine position compared to side sleeping. Some patients see their AHI drop from 25 to under 5 just by turning onto their side.
It’s not just about frequency. Supine sleeping also makes each event worse. Oxygen levels drop deeper, heart rates spike and dip more violently, and you wake up more often-even if you don’t remember it. That’s why you feel tired even after a full night’s sleep. Your body never gets deep, restorative rest.
Why Side Sleeping Works Better
Side sleeping keeps your airway open. Without gravity pulling your tongue backward, your throat stays clearer. Studies from the Sleep Foundation show side sleeping reduces snoring and apnea events more effectively than any other position. It’s not a cure, but for many, it’s enough to turn severe OSA into mild or even normal breathing patterns.
One study found that patients who slept only on their side reduced their nighttime breathing interruptions by 70%. That’s not a small improvement. It’s life-changing. People report better sleep quality, less morning headache, and more energy during the day. Their partners notice too-snoring often stops completely within seconds of a position change.
What Is Positional Therapy?
Positional therapy is any method that helps you avoid sleeping on your back. It’s not a new idea. For decades, people have sewn tennis balls into the back of their pajamas to make lying on their back uncomfortable. It’s cheap, simple, and surprisingly effective for some. But it’s not perfect. Many people wake up sore, frustrated, or just too uncomfortable to stick with it.
Modern positional therapy is smarter. Devices like the NightBalance Sleep Position Trainer (SPT) use gentle vibrations to nudge you back onto your side when you roll onto your back. They don’t wake you up-they just remind you. A 2015 study in the Journal of Clinical Sleep Medicine found that 68% of people using SPT achieved treatment success (AHI under 5), compared to just 43% using the tennis ball method. Compliance was over 30% higher with the device. People also reported better quality of life and higher satisfaction.

Comparing Methods: Tennis Ball vs. High-Tech Devices
| Method | Cost | Effectiveness | Compliance Rate | Comfort |
|---|---|---|---|---|
| Tennis Ball Technique | $0-$5 | Moderate | ~55% | Low |
| Specialized Side-Sleeping Pillow | $20-$50 | Moderate | ~60% | Medium |
| Wearable Vibration Trainer (e.g., NightBalance) | $300-$400 | High | ~85% | High |
| Smart Nora (Air Pressure System) | $500 | High | ~80% | High |
Most people who try the tennis ball method quit within three months. The discomfort is real. But the high-tech devices? They’re designed to work with your sleep, not against it. You barely notice the vibration. And because they’re quiet, your partner doesn’t even know it’s happening.
Who Should Try Positional Therapy?
Not everyone with sleep apnea benefits from positional therapy. It only works if your apnea is strongly linked to your sleep position. That’s called positional OSA. Doctors diagnose it by reviewing your sleep study data-specifically, comparing your AHI when you’re on your back versus your side. If your supine AHI is at least double your non-supine AHI, you’re a candidate.
Research shows that 50-60% of OSA patients have this pattern. Some groups, like people who are overweight or have mild to moderate apnea, are more likely to be positional. If your AHI is above 30 and you still have events on your side, positional therapy alone won’t be enough. You’ll likely need CPAP or another treatment.
But here’s the key: even if you need CPAP, positional therapy can still help. Many patients who struggle with CPAP adherence because it’s bulky or noisy find they can stick with a combination of CPAP and side sleeping. It reduces pressure needs and makes the machine work better.
Positional Therapy vs. CPAP
CPAP is still the gold standard. It’s more effective at lowering overall AHI. But adherence is the problem. Only about 50-60% of people use CPAP consistently for more than a year. With positional therapy, adherence rates jump to 80-90%. That’s huge. A treatment that works 90% of the time is better than one that works 100% of the time but is only used 50% of the time.
The American Academy of Family Physicians says positional therapy should be considered a first-line option for mild to moderate positional OSA. For people who hate CPAP, can’t tolerate it, or just want a simpler solution, it’s a powerful alternative. It’s not a replacement for everyone-but for the right person, it’s everything.
How to Get Started
First, get a sleep study that includes positional data. Most labs now track this, but ask your doctor to make sure. If your results show positional OSA, you have options:
- Start with a side-sleeping pillow. It’s low-cost and easy to try.
- If that doesn’t work, try the tennis ball trick for a week. See how your body reacts.
- If you’re still struggling, consider a wearable device. Look for FDA-cleared options like NightBalance or Smart Nora.
- Combine positional therapy with head elevation. Raising your head by 6-8 inches helps keep your airway open even more.
Give it at least two weeks. Your body needs time to adjust. Don’t expect overnight results. But if you stick with it, many people report feeling better within days.
What About Central Sleep Apnea?
Positional therapy works best for obstructive sleep apnea. For central sleep apnea-where your brain doesn’t send the right signals to breathe-side sleeping might help a little, but not as much. Researchers think it’s because central apnea is tied to brainstem function, not airway collapse. Still, some patients with mixed apnea (both types) benefit from side sleeping, especially if they have a strong positional component.
Final Thoughts
You don’t need to live with gasping nights and tired days. For a large group of people with sleep apnea, the solution is as simple as changing how you lie down. Positional therapy isn’t flashy. It doesn’t require surgery or a mask. It just asks you to sleep differently. And for many, that’s enough.
If you’ve been told you have sleep apnea but hate CPAP, or if your partner says you snore worse when you’re on your back, it’s worth exploring. Talk to your doctor. Get your sleep study reviewed for positional patterns. You might be surprised how much better you feel just by turning onto your side.
Can sleeping on my side cure sleep apnea?
For people with positional obstructive sleep apnea (POSA), side sleeping can reduce symptoms enough to bring AHI into the normal range. It’s not a cure for everyone, but it can eliminate the need for CPAP in mild to moderate cases. If your apnea happens regardless of position, side sleeping alone won’t be enough.
Is the tennis ball method still effective?
Yes, but only for short-term use. It works for about half of people who try it, but most quit within three months because it’s uncomfortable and disrupts sleep. Modern vibration devices are more effective and better tolerated, with compliance rates over 80%.
How do I know if I have positional sleep apnea?
You need a sleep study that breaks down your apnea-hypopnea index (AHI) by sleep position. If your AHI while on your back is at least twice as high as when you’re on your side, you have positional OSA. Ask your sleep specialist to review your positional data-it’s not always included by default.
Do I still need CPAP if I use positional therapy?
Not necessarily. If your AHI drops below 5 consistently with side sleeping and positional therapy, you may not need CPAP. But if your apnea is severe or happens in all positions, CPAP or another treatment will still be needed. Many people use both: positional therapy to reduce CPAP pressure and improve comfort.
Are there any risks to sleeping on my side?
No significant risks. Side sleeping is naturally healthy for most people. It reduces snoring, improves digestion, and helps with acid reflux. Some report shoulder or hip discomfort at first, but this usually resolves with time or by using a supportive pillow. It’s far safer than untreated sleep apnea.
