Heart disease kills more women than all forms of cancer combined. Yet most women still don’t realize it’s their biggest threat. In the U.S., about 307,000 women die from heart disease every year - that’s one in five. And yet, in 2019, only 44% of women knew it was the top cause of death for them. The problem isn’t just lack of awareness. It’s that heart disease in women doesn’t look like what you see in movies.
What Heart Attack Symptoms Look Like in Women
When people think of a heart attack, they picture someone clutching their chest, screaming in pain, collapsing on the sidewalk. That’s the male stereotype. For women, it’s often quieter, stranger, and far easier to ignore. Chest pain still happens - about 70% to 80% of women feel it during a heart attack. But it’s rarely the sharp, crushing pain men describe. Women more often report a dull pressure, tightness, or burning - like a heavy weight sitting on their chest. Sometimes it only shows up when they’re stressed, or wakes them up at night. The real red flags? Symptoms that have nothing to do with the chest at all.- Unexplained fatigue so bad you can’t make your bed - this happens in 71% of women who’ve had a heart attack.
- Shortness of breath during normal activities, like walking to the mailbox or climbing stairs.
- Pain in the jaw, neck, shoulder, or upper back - often described as a deep ache, not a sharp sting.
- Nausea, vomiting, or indigestion that comes out of nowhere.
- Dizziness, lightheadedness, or sudden sweating without exertion.
Why Women’s Hearts Are Different
Women don’t just have different symptoms. Their hearts and arteries work differently. Most heart attacks in men happen because a major artery gets blocked by plaque. In women, that happens too - but more often, the problem is in the tiny arteries that feed the heart muscle. This is called microvascular disease. It’s harder to detect with standard tests because those arteries are too small to show up on an angiogram. But the symptoms? Real. Fatigue. Breathlessness. Pain that comes and goes. Women are also more likely to experience conditions like:- SCAD (Spontaneous Coronary Artery Dissection): A tear in a heart artery, often triggered by extreme stress or pregnancy. It’s rare, but 80% of cases happen in women under 50 with no prior heart issues.
- Takotsubo syndrome (broken heart syndrome): A temporary heart condition triggered by intense emotional or physical stress. It mimics a heart attack, but there’s no blockage. It’s far more common in postmenopausal women.
The Silent Killer: Silent Heart Attacks
Some heart attacks in women happen without any noticeable symptoms at all. These are called silent heart attacks. About 34% of women over 65 have them - compared to 22% of men in the same age group. They don’t feel chest pain. They might just feel unusually tired for days, or have mild indigestion. Many don’t even realize it happened until an EKG years later shows scarring on the heart. That’s why routine checkups matter more than ever. If you’re over 50, especially if you’ve had pregnancy complications, early menopause, or a family history of heart disease, ask your doctor for a cardiac risk assessment - even if you feel fine.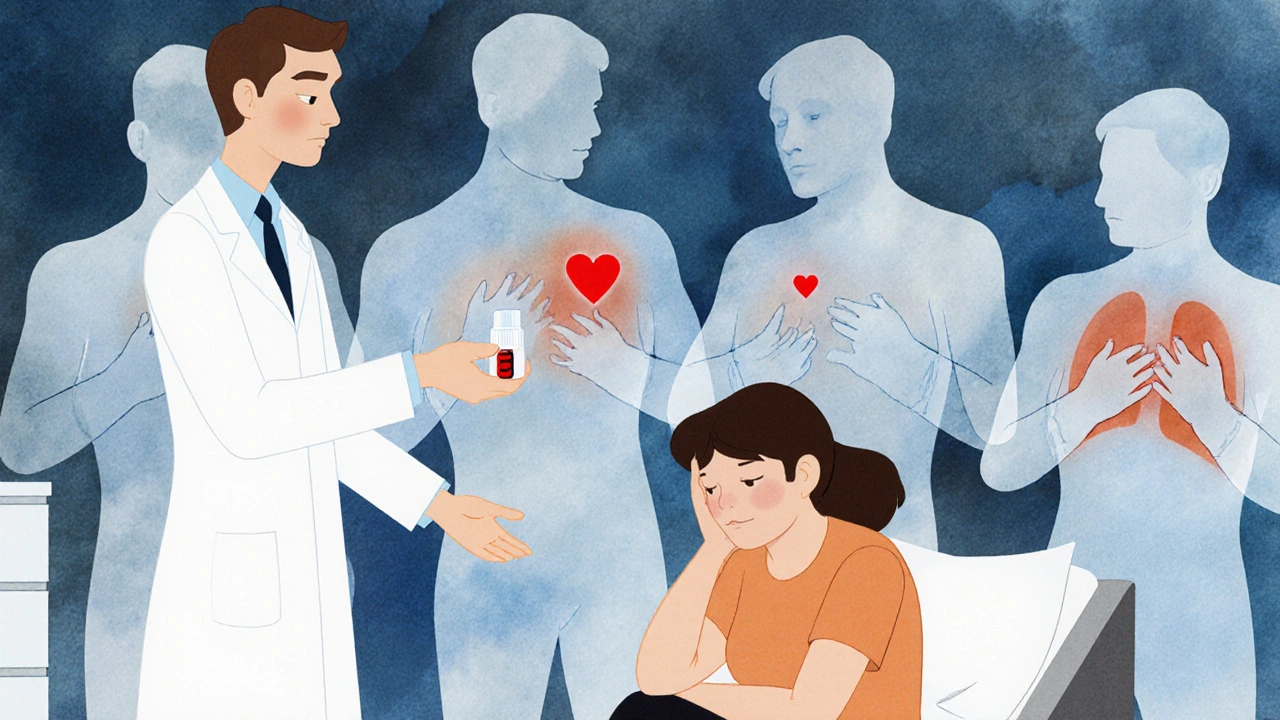
Why Doctors Miss It
It’s not just that women don’t recognize the signs. Doctors miss them too. A 2022 study in JAMA Internal Medicine found that in nearly 7 out of 10 emergency room cases where women had heart attack symptoms, doctors assumed they were anxious, depressed, or having a panic attack. Women are more likely to be told to “take an antacid” or “go home and rest.” Bias isn’t always intentional. But it’s real. For decades, heart research was done almost entirely on men. The Framingham Heart Study - the foundation of modern heart disease understanding - enrolled only men. Even today, women make up just 38% of participants in major cardiovascular trials. So the tools, tests, and training are still mostly built for male bodies.What You Can Do: Risk Management for Women
You can’t change your gender or your age. But you can change how you protect your heart. Track your history. Write down:- Any pregnancy complications (preeclampsia, gestational diabetes, preterm birth)
- Age when you went through menopause
- Family history of early heart disease (before age 55 for women, 45 for men)
- History of autoimmune conditions like lupus or rheumatoid arthritis
- Blood pressure (aim for under 120/80)
- Cholesterol (LDL under 100 mg/dL)
- Blood sugar (fasting under 100 mg/dL)
- Body weight (BMI under 25, waist under 35 inches)

When to Go to the ER
If you’re a woman and you experience three or more of these symptoms together - even if they’re mild - go to the ER immediately:- Unusual fatigue
- Shortness of breath
- Nausea or vomiting
- Jaw, neck, or back pain
- Lightheadedness or sudden sweating

Comments
vanessa parapar
Okay but let’s be real - if your doctor looks at you like you’re just ‘stressed’ after you say you’re exhausted and your jaw aches, they’re not just negligent, they’re dangerous. I had a silent heart attack at 48 and they sent me home with Tums. I didn’t know until my EKG showed scars two years later. This isn’t just awareness - it’s survival.
On November 21, 2025 AT 08:52
Ben Wood
Let me just say, as someone who’s read every peer-reviewed paper on cardiovascular pathology since 2012 - the Framingham study’s gender bias is not merely a ‘gap,’ it’s a catastrophic epistemological failure. The fact that microvascular disease remains underdiagnosed because angiograms are designed for male anatomy is not an oversight - it’s systemic misogyny masquerading as medical science. And don’t get me started on the FDA’s approval process…
On November 21, 2025 AT 22:20
Sakthi s
Good info. Stay active. Know your numbers. Your heart will thank you.
On November 23, 2025 AT 08:59
Rachel Nimmons
Did you know the pharmaceutical companies funded 92% of the early heart disease studies? And that’s why they still push statins for women even when the data shows minimal benefit. They don’t want us to know about the real causes - toxins, stress hormones, and the fact that our bodies aren’t just ‘small men.’
On November 24, 2025 AT 16:49
Abhi Yadav
we are all just stardust trying to keep our hearts beating in a world that refuses to see us as whole... the pain in the jaw? it's the soul screaming for recognition 🌌
On November 25, 2025 AT 04:32
Julia Jakob
they keep saying ‘women’s heart disease is different’ like it’s some cute little quirk instead of a medical emergency. i’ve been ignored by 3 doctors for ‘fatigue’ - turns out i had microvascular disease. they don’t teach this in med school because they’re still using 1970s textbooks written by men who thought women were ‘hysterical.’ if you’re tired, don’t nap - get tested. period.
On November 26, 2025 AT 05:40
Robert Altmannshofer
I’ve worked in ERs for 22 years and I’ve seen this over and over. A woman comes in with nausea, back pain, and cold sweats - we run the labs, do the EKG, and sure enough - it’s a heart attack. But the first thing the nurse says? ‘Did you eat something bad?’ It’s not malice. It’s habit. And habits kill. We need to retrain every single provider - from triage to attending - because if we don’t, we’re just doing the same thing and expecting different results.
On November 27, 2025 AT 23:36
Kathleen Koopman
sooo… if you’re a woman and you’ve ever thought ‘maybe i’m just tired’… stop. 🫀🩺 your body isn’t being dramatic - it’s screaming. i had a silent heart attack at 42 and didn’t know until my cardiologist said ‘your heart looks like it’s been through a war.’ please, please, please - get checked. even if you feel fine. ❤️
On November 29, 2025 AT 18:33
Nancy M
It is of paramount importance that societal norms surrounding the perception of female health be critically re-examined. The medical establishment's historical exclusion of women from clinical trials constitutes a profound ethical lapse. Furthermore, the normalization of fatigue and stress as benign female experiences perpetuates a dangerous paradigm that prioritizes convenience over clinical accuracy. One must advocate, with unwavering resolve, for equitable diagnostic protocols.
On December 1, 2025 AT 16:09
gladys morante
they told me it was anxiety. i cried for three days. then i went to a second doctor and they found a 90% blockage. i’m 45. i have two kids. i’m not ‘stressed’ - i’m dying and no one noticed. why do we have to fight just to be heard?
On December 3, 2025 AT 02:46
Precious Angel
Let me tell you something - this whole ‘women’s heart disease’ thing is a distraction. They don’t want you to know the real cause: glyphosate in your food, microplastics in your water, and the fact that your estrogen is being poisoned by corporate chemicals. The FDA doesn’t care - they’re paid off. The ‘Corus CAD test’? It’s just another way to make you pay for tests they should’ve been doing for decades. And don’t even get me started on how the ‘Women’s Cardiovascular Centers’ are just PR stunts while Big Pharma keeps selling statins to women who don’t need them. You’re being gaslit by the entire system.
On December 4, 2025 AT 12:40
Melania Dellavega
I used to think heart disease was something that happened to older men. Then my mom had a silent heart attack at 52 - no chest pain, just exhaustion. She didn’t know until her EKG showed scarring. I started tracking my numbers, walking every day, and speaking up when I felt off. It’s not about fear. It’s about knowing your body. You don’t have to be loud to be heard - just consistent. Your heart isn’t asking for perfection. It’s asking for attention.
On December 5, 2025 AT 04:16
Bethany Hosier
While I appreciate the data presented, I must emphasize that the narrative of systemic gender bias in cardiology is not universally supported by epidemiological evidence. Some studies indicate that when controlling for comorbidities and presentation severity, diagnostic accuracy between genders converges. Furthermore, the notion that ‘women’s hearts are different’ may inadvertently reinforce biological essentialism rather than promote equitable care. Perhaps the focus should be on individualized risk assessment rather than gendered assumptions - even if those assumptions are well-intentioned.
On December 5, 2025 AT 15:01