Akathisia vs. Restless Legs Symptom Checker
How can you tell if your restlessness is akathisia or restless legs?
This tool helps you distinguish between akathisia (a medication-induced movement disorder) and restless legs syndrome (RLS) based on your symptoms and medication history.
1. When do your symptoms occur?
2. Where do you feel the discomfort?
3. How would you describe the sensation?
4. What medications are you currently taking?
5. How does movement affect your symptoms?
When you start a new medication-especially an antipsychotic-you expect relief from hallucinations, paranoia, or severe anxiety. You don’t expect to feel like you’re being pushed out of your own skin. But for many people, that’s exactly what happens. A deep, unshakable urge to move, especially in the legs, that doesn’t go away no matter how much you pace, shift, or stretch. It’s not laziness. It’s not anxiety. It’s not just being fidgety. It’s akathisia-a medication-induced movement disorder that’s dangerously easy to miss.
What Is Akathisia, Really?
Akathisia isn’t just feeling restless. It’s a physical and emotional torment. People describe it as an internal burning, aching, or crawling sensation that forces them to move. You can’t sit still. You can’t relax. Even when you’re exhausted, your body demands motion. You cross and uncross your legs repeatedly. You rock back and forth. You pace in place. You stand up just to sit down again. The movement doesn’t bring relief-it’s the only thing that keeps the discomfort from exploding. This isn’t rare. About 20-40% of people taking older antipsychotics like haloperidol develop akathisia. Even newer drugs like risperidone cause it in up to 14% of users. The symptoms usually show up within days to weeks after starting or increasing the dose. That’s why doctors often don’t connect the dots: they see a patient who’s “more agitated,” and they think the psychosis is worsening. So they increase the dose. And the akathisia gets worse. And worse. And worse. In one documented case, a patient on haloperidol was told his restlessness was “just anxiety.” His dose was doubled. Within days, he developed suicidal thoughts. Only after stopping the drug-and starting a low dose of clonazepam-did he feel like himself again. That’s not an outlier. Studies show akathisia is linked to suicidal ideation, aggression, and violence. And it’s misdiagnosed in up to half of cases.How Is Akathisia Different From Restless Legs Syndrome?
Many people confuse akathisia with restless legs syndrome (RLS). Both involve leg discomfort and an urge to move. But they’re not the same. RLS happens mostly at night or during rest. It feels like tingling, crawling, or pulling deep in the legs. Moving helps-walking around eases the feeling. People with RLS often have low iron, a family history, or kidney disease. Treatment? Iron supplements, dopamine-boosting drugs like levodopa, or gabapentin. Akathisia is different. It happens anytime you’re sitting or standing still. It’s not just in the legs-it’s in your whole body. You feel it in your chest, your arms, your torso. It’s not a tingling. It’s a crushing, urgent need to move. And movement doesn’t relieve it-it just distracts from it for a moment. Crucially, akathisia starts after taking certain medications. RLS doesn’t. Here’s the kicker: drugs that help RLS, like levodopa, can make akathisia worse. And drugs that help akathisia, like propranolol or clonazepam, do nothing for RLS. Mixing them up leads to the wrong treatment-and worse symptoms.Which Medications Cause Akathisia?
The biggest culprits are antipsychotics. First-generation ones like haloperidol, fluphenazine, and chlorpromazine carry the highest risk. They block dopamine hard and fast, which is why they work for psychosis-but also why they trigger akathisia. Second-generation antipsychotics like risperidone, olanzapine, and quetiapine are better, but still risky. About 5-15% of people on these drugs develop akathisia. Even antidepressants like SSRIs (sertraline, fluoxetine) and anti-nausea meds like metoclopramide can cause it. The key trigger? Dopamine blockade. Any drug that strongly blocks dopamine receptors in the brain can cause akathisia. That’s why newer drugs like lumateperone (Caplyta) are designed to avoid that. In clinical trials, it caused akathisia in only 3.6% of users-far lower than risperidone’s 14.3%.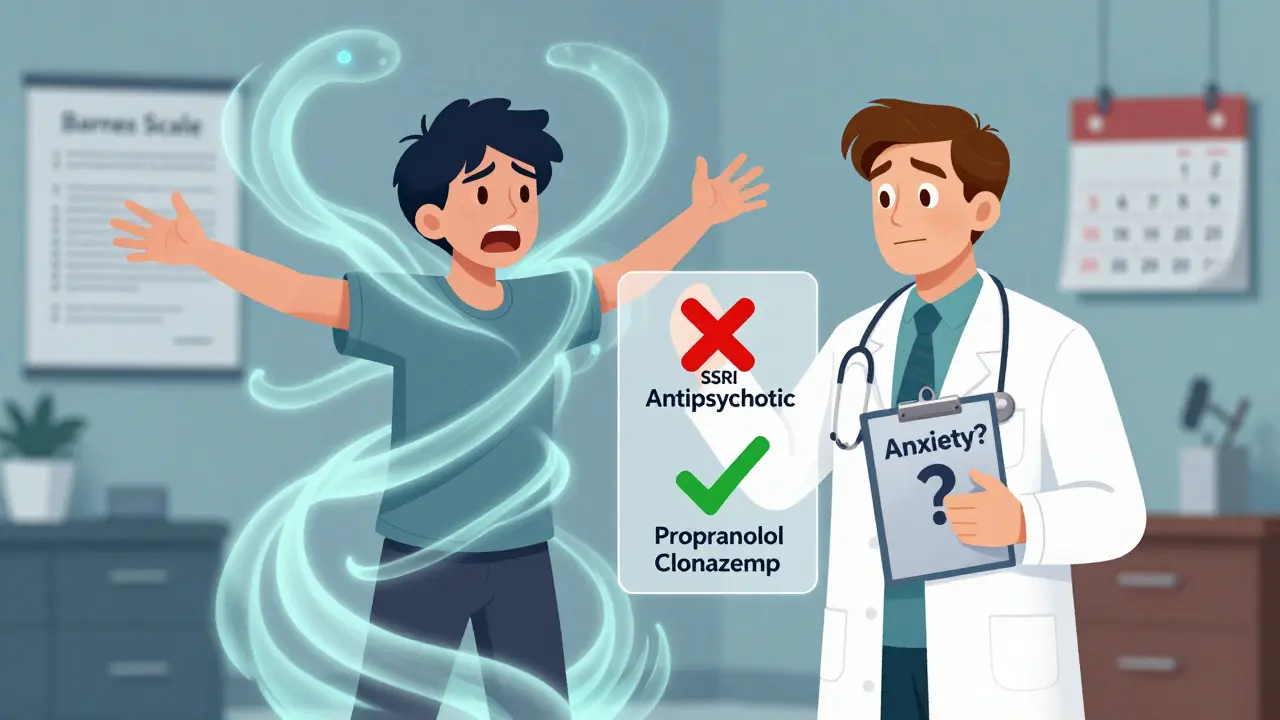
How Do Doctors Diagnose It?
There’s no blood test. No scan. No single symptom that screams “akathisia.” Diagnosis relies on two things: asking the right questions and watching closely. The Barnes Akathisia Rating Scale (BARS) is the gold standard. It takes 5-10 minutes. The doctor asks: “Do you feel an inner restlessness that makes you feel like you have to move?” Then they observe: Are you shifting your weight? Crossing and uncrossing your legs? Pacing? Rocking? Are you unable to sit still for more than a few seconds? They also rule out other movement disorders. Parkinsonism? That’s tremors, stiffness, slow movement. Tardive dyskinesia? That’s involuntary lip-smacking, tongue protrusion, or finger twitching. Akathisia is pure, urgent motion-no tremors, no tics. Just the unbearable need to move. Too often, primary care doctors don’t know this. They hear “I can’t sit still,” and they prescribe an anti-anxiety pill. That’s like treating a broken leg with painkillers. The problem stays. The damage grows.What’s the Best Treatment?
The first rule? Stop or reduce the drug causing it-if you can. If it’s haloperidol, tapering it over 3 days often makes symptoms vanish. In one case, a patient went from unbearable restlessness to feeling “back to myself” in 72 hours. That’s not magic. That’s removing the trigger. But what if you can’t stop the antipsychotic? Your psychosis is too severe? Then you add a treatment that targets akathisia directly. - Propranolol: A beta-blocker. Start with 10 mg twice daily. It reduces the physical urge to move. Works for about 60% of patients. - Clonazepam: A benzodiazepine. 0.5 mg at night. Calms the nervous system. Helps with sleep and inner tension. - Cyproheptadine: An antihistamine with serotonin-blocking effects. 4 mg daily. Less commonly used, but effective in some cases. Newer options are coming. Pimavanserin (Nuplazid), originally for Parkinson’s psychosis, showed 62% reduction in akathisia in a 2023 trial. Transcranial magnetic stimulation is being tested at Harvard. And AI tools are being developed to detect akathisia from video calls-using subtle movement patterns to flag it before the patient even speaks.Why Is This So Often Missed?
Because it’s invisible. You don’t look sick. You don’t have a fever. You don’t have a rash. You’re just… restless. And in a world that’s already overwhelmed with mental health crises, doctors don’t always have time to dig deeper. A 2022 survey by NAMI found that 68% of antipsychotic users who had restlessness symptoms were told it was “just anxiety.” And 42% of those people had their medication increased-making things worse. It’s not just ignorance. It’s systemic. Most electronic health records don’t have a checkbox for akathisia. No automated alerts. No training modules for primary care providers. Only 37% of U.S. psychiatric facilities routinely screen for it. The result? People suffer for months. Some quit their meds. Some end up in the ER. Some die by suicide.
What Should You Do If You Think You Have It?
If you’re on an antipsychotic-or any medication that affects dopamine-and you feel this inner torment, don’t wait. Don’t assume it’s “in your head.” - Write down your symptoms: When do they start? When do they get worse? What makes them better or worse? - Track your medication changes: Did this start after a dose increase? After switching drugs? - Bring the Barnes Scale info with you. Print it. Show your doctor. Say: “I think this might be akathisia.” - Ask: “Could this be caused by my medication? Could we try lowering the dose or adding propranolol?” You’re not overreacting. You’re not dramatic. You’re describing a real, documented, dangerous side effect that’s been ignored for decades.The Bigger Picture
Akathisia isn’t just a side effect. It’s a warning sign. It’s the body screaming that something’s wrong with the treatment plan. And if we keep treating the symptom as the disease, we’re not helping-we’re harming. Newer antipsychotics are safer. Screening tools are getting better. Awareness is slowly rising. But until every doctor knows how to spot akathisia, people will keep suffering in silence. The good news? When it’s recognized, it’s often reversible. No lifelong disability. No brain damage. Just a medication adjustment-and a chance to breathe again.Frequently Asked Questions
Can akathisia go away on its own?
Sometimes, yes-if the medication is stopped or lowered. In many cases, symptoms improve within days to weeks after reducing the dose. But if the drug continues, akathisia can become chronic or even permanent. Waiting for it to “go away” without action is risky. It can worsen and lead to serious consequences like suicidal thoughts.
Is akathisia the same as anxiety?
No. While both can cause restlessness, anxiety is a mental state-fear, worry, racing thoughts. Akathisia is a physical movement disorder triggered by medication. People with akathisia feel an uncontrollable urge to move, even if they’re not anxious. In fact, many report feeling calm mentally but physically trapped. Treating it with anti-anxiety drugs often makes it worse.
Can antidepressants cause akathisia?
Yes. SSRIs like sertraline, fluoxetine, and escitalopram are known to cause akathisia, especially when started or increased. It’s less common than with antipsychotics, but still occurs in up to 10% of users. If you develop sudden restlessness after starting an antidepressant, don’t assume it’s just “adjusting.” Ask your doctor about akathisia.
Why doesn’t my doctor know about akathisia?
Many doctors, especially primary care providers, aren’t trained to recognize movement disorders. Akathisia isn’t taught in medical school the way diabetes or high blood pressure is. It’s often lumped under “anxiety” or “agitation.” But awareness is growing. Resources like the Barnes Scale and new AI tools are helping. If your doctor seems unsure, ask for a psychiatric consultation.
Are there any natural remedies for akathisia?
There’s no proven natural cure. Magnesium, vitamin B6, or herbal supplements like valerian root might help with general restlessness, but they won’t fix akathisia caused by dopamine-blocking drugs. The only reliable treatments are adjusting the medication or using proven drugs like propranolol or clonazepam. Don’t delay treatment hoping for supplements to work.
