Steroid Eye Risk Calculator
Your Risk Assessment
Results
Enter your information to see your risk assessment
Your Risk Level
Key Information
2 weeks: Risk begins to develop
4 weeks: Eye pressure starts rising in susceptible people
35%: Risk of glaucoma in people with no prior eye history
Permanent damage: Occurs if high pressure persists beyond 3 months
When you take steroids for asthma, arthritis, or an autoimmune condition, you’re usually focused on how much better you feel-less pain, easier breathing, fewer flare-ups. But there’s a silent side effect that can sneak up on you: steroid-induced eye damage. Two of the most serious risks? Cataracts and glaucoma. And they don’t wait years to show up. They can start forming in as little as two weeks of use.
How Steroids Attack Your Eyes
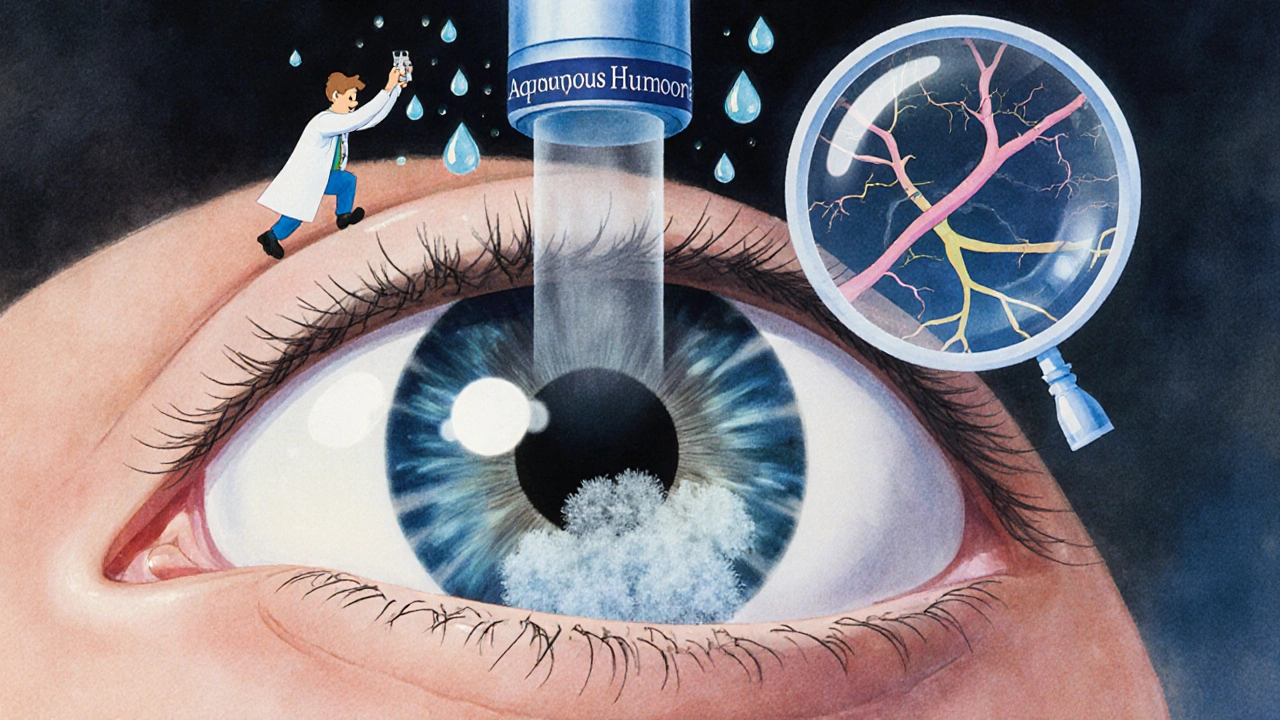
Steroids don’t just calm inflammation in your lungs or joints. They also change how your eyes work. The problem starts with the fluid inside your eye-the aqueous humor. Normally, it flows in and out smoothly, keeping pressure balanced. But steroids clog the drainage system. That’s what raises your eye pressure. And when pressure builds up for too long, it crushes the optic nerve. That’s glaucoma.For cataracts, steroids mess with the lens. They cause proteins to clump together in the back of the lens, creating a cloudy patch called a posterior subcapsular cataract. Unlike age-related cataracts that grow slowly, these develop fast. You might not notice until your vision suddenly turns blurry, colors look washed out, or headlights at night create halos.
It doesn’t matter if you’re taking steroids as a pill, an inhaler, a shot, or eye drops. All forms can cause damage. But eye drops? They’re the fastest route. A single drop every day for months can be enough to trigger changes. That’s why people using steroid drops for uveitis or after eye surgery are at the highest risk.
Who’s Most at Risk?
Not everyone who takes steroids gets eye problems. But some people are far more likely to. About 5% of the population is highly sensitive-called “steroid responders.” Their eye pressure jumps 15 mmHg or more with even small doses. Another 30% see a moderate rise. That means nearly one in three people could be at risk.High-risk groups include:
- People with a family history of glaucoma
- Those already diagnosed with glaucoma (up to 90% become steroid responders)
- Patients with diabetes or high myopia (nearsightedness)
- Anyone on steroid therapy for more than 2-4 weeks
- Post-cataract surgery patients on steroid eye drops
Here’s the scary part: nearly 35% of steroid-induced glaucoma cases happen in people with no prior eye history. No symptoms. No warning. Just a routine eye exam that reveals damage already done.
What Does the Damage Look Like?
Steroid-induced cataracts and glaucoma don’t always cause pain. That’s why they’re so dangerous.Cataract symptoms:
- Blurry or foggy vision, like looking through a frosted window
- Colors seem dull or yellowed
- Glare or halos around lights, especially at night
- Frequent changes in glasses prescription
- Difficulty seeing in low light
Glaucoma symptoms (often late-stage):
- Loss of peripheral vision (tunnel vision)
- Eye pain or redness (less common with steroid glaucoma)
- Seeing rainbow-colored rings around lights
- Sudden vision loss (rare, but possible if pressure spikes fast)
Many people don’t notice anything until their vision drops to 20/80 or worse. One patient in Leeds, on long-term prednisone for asthma, didn’t realize her vision had deteriorated until her optometrist found advanced cataracts during a routine check. She had no symptoms-just a slow, silent decline.
How Fast Does It Happen?
Timing matters. Steroid-induced eye damage doesn’t wait for years.- 2-4 weeks: Risk of cataract formation begins
- 4-8 weeks: Eye pressure starts rising in susceptible people
- 3-6 months: Significant risk of permanent optic nerve damage if pressure stays high
- 12+ months: Cataracts often require surgery; glaucoma may need lifelong treatment
Studies show that after 4 months of continuous steroid use, the chance of posterior capsular opacification (a type of cataract) jumps dramatically. And unlike age-related cataracts, these don’t stabilize-they keep getting worse.
Can It Be Reversed?
The good news? Eye pressure from steroids usually drops back to normal once you stop the medication. In most cases, if caught early, the pressure spike can be managed with eye drops that lower IOP.But here’s the catch: if high pressure lasts too long, it kills optic nerve cells. And those cells don’t come back. Once you lose peripheral vision or have optic nerve scarring, it’s permanent. That’s why timing is everything.
Cataracts caused by steroids don’t go away on their own. They need surgery. And because they’re dense and located in the back of the lens, they’re harder to remove than typical age-related cataracts. Recovery takes longer. The risk of complications is higher.
What Should You Do?
If you’re on steroids for more than two weeks, you need an eye exam. Not “maybe.” Not “when I have time.” Now.Here’s the step-by-step plan:
- Baseline exam: Get your eye pressure checked and your optic nerve imaged before starting steroids.
- First follow-up: At 2 weeks after starting steroids.
- Regular checks: Every 4-6 weeks for the first 3 months.
- Long-term: Every 6 months if you’re still on steroids, even if pressure is normal.
Ask your doctor for a referral to an ophthalmologist-not just your optometrist. You need someone who can measure pressure accurately, scan your optic nerve, and spot early signs of damage.
Also, ask: “Is there a non-steroid alternative?” For some conditions, drugs like loteprednol etabonate (a weaker steroid) or non-steroidal anti-inflammatories (NSAIDs) can work with much lower eye risk. New research shows these alternatives reduce IOP spikes by up to 70%.
What If You’ve Already Been on Steroids for Months?
If you’ve been on steroids for longer than 3 months and haven’t had an eye exam, don’t panic. But do act now.Book an appointment with an ophthalmologist. Tell them exactly how long you’ve been on steroids and what form you’re using. Bring a list of your medications. They’ll check your eye pressure, take images of your optic nerve, and scan your lens for cataracts.
If damage is found, treatment options include:
- Glaucoma eye drops to lower pressure
- Laser treatment to improve fluid drainage
- Surgery to remove steroid-induced cataracts
The sooner you act, the better your chances of keeping your vision.
Why Doctors Miss This
Here’s the broken part of the system: most primary care doctors don’t think to warn patients about eye risks. A study by the American Academy of Ophthalmology found that only 42% of doctors refer long-term steroid users for eye exams-even though guidelines have been clear for over a decade.Patients assume their doctor told them everything. Doctors assume someone else is handling it. The result? Thousands of people lose vision they never knew they were at risk for.
Don’t wait for someone else to protect your eyes. Be your own advocate. If you’re on steroids, say: “I need an eye exam. I’ve heard steroids can damage vision.”
The Bigger Picture
Steroids save lives. They’re essential for people with severe asthma, lupus, or after organ transplants. But they’re not harmless. The numbers are growing. In the U.S. alone, over 12 million steroid eye drop prescriptions are filled each year. More than 3 million adults take oral steroids long-term.These drugs cause 10-20% of all secondary glaucoma cases-and 5-10% of cataract surgeries in people under 55. That’s not rare. That’s common. And it’s preventable.
New tools are emerging. Genetic tests can now predict who’s likely to be a steroid responder with 85% accuracy. Home IOP monitors let patients track pressure between visits. Tele-ophthalmology programs are already helping veterans and rural patients stay protected.
But none of this matters if you don’t know to ask.
Final Warning
Steroid-induced eye damage doesn’t come with a warning label you can feel. No pain. No redness. Just slow, silent vision loss.It’s not a side effect you can ignore. It’s a silent emergency.
If you’re on steroids for more than two weeks, get your eyes checked. Don’t wait for symptoms. Don’t assume you’re fine. Your vision is worth more than a missed appointment.
And if you’ve already lost some vision? It’s not too late to stop further damage. But you need to act-today.

Comments
Shawna B
Got on prednisone for asthma last year and never thought about my eyes. Just got my first eye exam in 5 years and they found early cataracts. Scary how fast it happened. I’m getting checked every 3 months now.
On November 29, 2025 AT 02:31
Jerry Ray
Yeah right like steroids are the real problem. The real issue is Big Pharma pushing these drugs so they can sell you eye drops and surgeries. They don’t want you to know about natural anti-inflammatories like turmeric or CBD. The system is rigged.
On December 1, 2025 AT 02:25
David Ross
Let’s be clear: this is a catastrophic failure of medical oversight. The FDA has known about steroid-induced glaucoma since 1987. The American Medical Association has issued guidelines. Yet, 58% of primary care physicians still fail to refer patients for baseline ocular screening. This isn’t negligence-it’s malpractice. And the fact that you’re reading this means you’re one of the lucky ones who didn’t lose vision yet. Wake up.
On December 2, 2025 AT 02:38
Sophia Lyateva
steroids are a gov mind control tool to make you blind so they can put chips in your eyes lol. i heard it from a guy on youtube who used to work for the cia. my aunt’s optometrist said the same thing. they’re testing on us. dont trust the drs.
On December 3, 2025 AT 13:46
AARON HERNANDEZ ZAVALA
I’ve been on low-dose steroids for psoriasis for over a year. I didn’t know any of this. Thanks for laying it out so clearly. I’m scheduling my eye exam tomorrow. No excuses. We all need to look out for each other.
On December 5, 2025 AT 00:57
Lyn James
It’s not just about the steroids-it’s about the moral decay of modern medicine. We’ve turned human bodies into disposable machines. You don’t treat inflammation with chemicals-you treat it with discipline, fasting, sunlight, and spiritual alignment. But no, we’d rather pump poison into your veins and then sell you a $3000 lens implant. Your soul is not a pharmacy receipt. Your eyes are not a warranty claim. Stop outsourcing your health to corporations that profit from your blindness.
On December 5, 2025 AT 05:50
Craig Ballantyne
The clinical evidence is robust. Steroid-induced intraocular pressure elevation is well-documented in peer-reviewed ophthalmology literature. The risk stratification is clear: high responders exhibit a >15 mmHg increase within 2–4 weeks. Screening protocols are cost-effective and endorsed by NICE and AAO guidelines. The gap lies in implementation-not evidence. Primary care providers require better decision support tools and mandatory continuing education in ocular pharmacology.
On December 5, 2025 AT 22:05
Victor T. Johnson
Bro. I’ve been on prednisone for 18 months. No eye exam. Zero. I just found out my pressure is 32. I’m not mad. I’m just done. 😔👁️🗨️ I’m getting laser treatment next week. If you’re reading this and you’re on steroids-do it now. Don’t be me.
On December 6, 2025 AT 13:58
Nicholas Swiontek
Thank you for posting this. I’m a nurse and I’ve seen too many patients lose vision because they didn’t know. I’m sharing this with every patient on long-term steroids. You’re not just saving eyes-you’re saving lives. Keep speaking up 💪👁️
On December 7, 2025 AT 21:05
Robert Asel
It is patently incorrect to suggest that steroid-induced cataracts are reversible upon cessation of therapy. The literature demonstrates that while intraocular pressure may normalize, posterior subcapsular opacification is a structural alteration of lens proteins that persists indefinitely. Surgical intervention is the only definitive treatment. Furthermore, the assertion that 35% of cases occur in patients with no prior ocular history is misleading; many of these patients have undiagnosed genetic predispositions. The data must be interpreted with precision.
On December 9, 2025 AT 03:41
Shannon Wright
To everyone reading this: you are not alone. If you’re scared, that’s okay. If you’ve been putting off the eye exam, it’s not too late. I was diagnosed with steroid-induced glaucoma after 6 months on a biologic. I thought I was fine. I wasn’t. But because I listened-to my body, to this post, to my optometrist-I caught it early. I’m on eye drops. My vision is stable. You can do this. One step. One call. One appointment. Your eyes are worth it. I believe in you.
On December 10, 2025 AT 18:20
vanessa parapar
Wow. I’ve been using steroid eye drops for dry eyes for 2 years. I thought it was safe because it’s just drops. You’re right-I’m a dumbass. I’m booking an appointment right now. Thanks for the wake-up call. 🙏
On December 11, 2025 AT 20:18
Ben Wood
What’s truly appalling is that this isn’t even controversial. The mechanisms are textbook. The timelines are published. The risk factors are quantified. And yet, the medical establishment continues to treat this as an afterthought. This isn’t oversight-it’s systemic incompetence. And the fact that you’re still reading this means you’re one of the few who still care enough to act. Shame on the rest.
On December 12, 2025 AT 08:08